NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
National Guideline Alliance (UK). Cerebral palsy in under 25s: assessment and management. London: National Institute for Health and Care Excellence (NICE); 2017 Jan. (NICE Guideline, No. 62.)
G.1. Literature review
The search strategies described in Appendix E identified 1,175 papers. Once the screening of titles and abstracts was complete, 1 full version of a selected paper was acquired for assessment using the methods described in Section 3.3.6 ‘Evidence of cost-effectiveness’. However this paper was a study protocol and subsequently excluded. Overall, none of the 1,175 papers identified from the search were considered to be relevant to the review questions in this guideline. Figure 1 below provides an illustration of the process used to select those papers.
G.2. Assessment of eating, drinking and swallowing difficulties
G.2.1. Literature review
No economic evaluations of videofluoroscopic swallow studies (VF) or fibreoptic endoscopic evaluation of swallowing (FEES) in children and young people with cerebral palsy were identified in the literature search conducted for this guideline.
G.2.2. Background and methods
Performing VF or FEES in addition to a clinical assessment will incur additional resources; neither diagnostic procedure would be considered cost-effective if there is not an effective treatment for the condition being diagnosed, or if the patient’s management is not changed by the results. In other words, if VF or FEES do not add any additional information to a clinical assessment and do not change the patient’s management strategy, VF and FESS should not be recommended.
The clinical evidence review identified 1 study (DeMatteo 2005) with a mixed population of children with different conditions that compared clinical assessment to VF and 1 study (Beer 2014) that compared clinical assessment to FEES in 5 participants with cerebral palsy. Both studies failed to demonstrate the usefulness of clinical assessment to rule in or rule out swallowing difficulties above the reference test (VF or FEES). What it did not show was the level of information that VF or FEES shows beyond routine clinical assessment. Despite this low quality evidence, the Committee agreed VF and FEES can provide information about different stages of swallowing which is challenging to accurately gain from a clinical assessment. For example, information on whether the bolus is refluxing to the nasal space, how efficiently the pharynx is cleared after swallowing, how effectively the child clears aspirated material from the airway, or if the child or young person with cerebral palsy is silently aspirating. Also, if the child or young person with cerebral palsy silently aspirates during VF or FEES this might be treated differently to clinical assessment alone. In light of this additional information, their management may change leading to an improvement in their quality of life, potentially justifying the costs of the procedure.
However, the effectiveness of VF and FEES can be compromised as the ability to swallow can be influenced by several factors such as the person’s position and noise that may be difficult to control during the procedure. As a result the child or young person with cerebral palsy may not obviously aspirate during VF or FEES, even when clinical observation and history are strongly suggestive of aspiration. According to the Committee these would be false negatives with regards to the test, if taken in isolation, but taking into account all aspects of history and examination this would not mean that they would not be treated for swallowing difficulties. In this instance, the cost-effectiveness of VF and FESS is questionable, particularly if the patient’s management strategy is unchanged by the results of the procedure.
The Committee also highlighted that VF and FEES can overestimate the severity of swallowing difficulties for the reasons outlined above. This could lead to over-treatment which, at worst, could include gastrostomy placement or, more likely, implementation of strategies to reduce aspiration risk by making dietary changes. Gastrostomy is a relatively expensive and invasive intervention to manage difficulties with eating, drinking and swallowing. This procedure also has potential to have a negative impact on the child or young person’s quality of life, particularly in terms of social interaction and satisfaction from eating.
Given that many paediatric departments do not have the necessary competencies to perform VF or particularly FEES, recommendations in favour of VF or FEES could lead to implementation costs. To aid considerations of cost-effectiveness, a cost description was undertaken.
G.2.3. Resource and cost use
G.2.3.1. Videofluoroscopic swallow studies (VF)
According to the Committee, VF is readily available in hospitals with an adult speech and language service, but in fewer paediatric departments. One reason is limited access to paediatric speech and language therapists (SLTs) with the necessary competencies to perform VF. Occasionally, paediatric VFs are carried out by the adult SLT department, but with a paediatric SLT in attendance.
Table 1 below presents the national average unit cost of a VF outpatient procedure performed by an imaging service. The Committee noted that there are difficulties in using both VF and FEES in children due to compliance, positioning, availability and level of team expertise, but this is not limited to children with cerebral palsy. The Committee advised that a paediatric centre would undertake at least 20 VF procedures a week, but this would be much greater in adults. For this reason, a procedure with a duration of more than 40 minutes, and a duration of 20 to 40 minutes, could be considered as proxies for children and adults, respectively.
Table 1Cost of VF
| Currency description | National Average Unit Cost | Source |
|---|---|---|
| Contrast Fluoroscopy Procedures with duration of more than 40 minutes | £256 | NHS Reference Costs 2014/15, IMAGDA, RD32Z |
| Contrast Fluoroscopy Procedures with duration of 20 to 40 minutes | £149 | NHS Reference Costs 2014/15, IMAGDA, RD31Z |
According to the Committee the optimal procedure would involve a radiographer (to obtain the images), radiologist and SLT to interpret the images. Although in some centres, interpretation can be performed solely by the radiologist or SLT. If no radiographer is present then the radiologist would be the operator of the equipment.
The Committee highlighted that there is variable practice across the country surrounding the health care professionals involved during the procedure. This was demonstrated by the Glasgow Royal Infirmary Hospital (cost year 2009) who compared a VF clinic staffed by SLTs and radiographers to consultant radiologists and SLTs. They found a SLT led procedure was more time efficient and gave a more comprehensive assessment of swallowing dangers. This clinic arrangement meant that the cost of a VF was reduced from £345 (using a consultant radiologist and SLT) to £215 (using a radiographer and SLT).
G.2.3.2. Fibreoptic endoscopic evaluation of swallowing (FEES)
According to the Committee, FEES is readily available in hospitals with an adult Ear, Nose and Throat (ENT) service, but used much more rarely than VF in paediatric departments. Most procedures are performed by an ENT specialist and SLT. Similarly to VF, a third health care professional may also be present to operate the equipment, but practice is variable across the country. The Committee noted that children may require a general anaesthetic and overnight stay; hence, Table 2 below presents the cost of a FEES procedure in an outpatient setting and inpatient setting. The Committee also noted that FEES is rarely performed, questioning the reliability of the cost in Table 2 in children and young people with cerebral palsy to assess eating, drinking and swallowing difficulties.
Table 2Cost of FEES
| Currency description | National Average Unit Cost | Source |
|---|---|---|
| Diagnostic Endoscopic Upper Gastrointestinal Tract Procedures, 19 years and over, outpatienta | £239 | NHS Reference Costs 2014/15, ENT service code 120, FZ60Z |
| Diagnostic Endoscopic Upper Gastrointestinal Tract Procedures, 19 years and over, elective inpatienta | £901 | NHS Reference Costs 2014/15, FZ60Zb |
ENT, Ear, Nose and Throat
- a
Costs not reported for Diagnostic Endoscopic Upper Gastrointestinal Tract Procedures in patients under 19 years
- b
ENT service not specified for inpatient procedures
G.2.4. Conclusions
The Committee’s view was that VF and FEES can provide additional information to clinical assessment. However, clinical assessment would be the first line in any decision making, because the results from a VF or FEES would not be taken in isolation; questioning the cost-effectiveness of routine VF or FEES without specific clinical concern.
Moreover, if children and young people with cerebral palsy have difficulties tolerating the procedure the quality of the results obtained from a VF and FEES could be compromised, potentially reducing their clinical and cost-effectiveness in addition to a standardised assessment.
The Committee’s discussion regarding the associated economic benefits and harms are reported in Section 12.4.3 ‘Evidence to recommendations’.
G.3. Management of eating, drinking and swallowing difficulties
G.3.1. Literature review
No economic evaluations of interventions to manage eating, drinking and swallowing difficulties were identified in the literature search conducted for this guideline.
G.3.2. Background and methods
This review question was not prioritised for de novo economic modelling. However the interventions under consideration are likely to be given by a speech and language therapist (SLT), occupational therapist (OT) or physiotherapist, and staff time can be of high cost. Also the frequency and content of the interventions may vary and the Committee highlighted that there is currently variable delivery across the country. For these reasons, relevant resource and cost use data are presented to aid consideration of cost-effectiveness.
G.3.3. Resource and cost use
G.3.3.1. Feeding equipment
Most modifications with regards to feeding equipment involve changes to the size or shape of cutlery. However, some children and young people with cerebral palsy may require more high-tech electro/mechanical assistive devices if those modifications prove to be ineffective.
The Committee advised that the Neater Eater is the most commonly used high-tech assistive device in the UK and if such devices are considered a success, they would be used on an ongoing basis – potentially over a person’s lifetime.
Regardless of the specific model, each child or young person with cerebral palsy would receive their own personalised assistive device. These types of devices would generally be used as part of daily life in the same way that we would use cutlery.
Following a successful trial of the device, the child or young person with cerebral palsy and their families or carers would be trained by a company representative, OT and/or SLT over several home visits.
The upfront capital cost of a Neater Eater is relatively expensive at a cost of approximately £2,900 according to the manufacturer. Ideally the device would undergo annual reviews with a SLT at the child or young person’s home where it is most frequently used.
Neater Eaters have a 3 year warranty although the device is expected to last longer than this. The manufacturer offers a refurbishment package for units less than 7 years old that replaces ropes, drive belt, power supply, switches, plates and cutlery and includes a further 12 month warranty (if purchased outside of the original 3 year warranty) and a set up visit from one of their demonstrators. The refurbishment package costs £843 plus value added tax (VAT).
Purchasing an electro/mechanical assistive device is a capital cost, requiring an up-front payment. There are 2 aspects to capital costs:
- opportunity cost – this is the money spent on the device that could have been invested in another venture. This cost is calculated by applying an interest rate on the sum invested in the capital;
- depreciation cost – the device has a certain lifespan and depreciates over time, and will eventually need to be replaced.
The usual practice for economic evaluation is to calculate an ‘annual equivalent cost’. This is calculated by annuitizing the initial capital outlay (including staff/training costs) over the expected life of the device. Calculating the equivalent annual cost means making allowance for the differential timing of costs by discounting.
The formula for calculating the equivalent annual cost is:
Where:
- E = equivalent annual cost
- K = purchase price of the device
- T = training
- S = resale value
- r = discount (interest) rate
- n = device lifespan
- A(n,r) = annuity factor (n years at interest rate r)
Using this formula a cost per person per annum for use of an electro/mechanical assistive device was calculated to allow for comparison.
Table 3 below presents the parameters used to calculate the equivalent annual cost of an electro/mechanical assistive device.
Table 3Annual cost of an electro/mechanical assistive device
| Parameter | Value | Source |
|---|---|---|
| K = purchase price of a electro/mechanical device (excluding VAT) | Device, £2,900; refurbishment package, £843 | According to the Neater Eater manufacturer, the price of their Electric Programmable Neater Eater (NE-GCE) is £2881 plus delivery and VAT. Assuming a delivery cost of approximately £20 the purchase price has been uplifted to £2,900. The manufacturer also offers a refurbishment package for units less than 7 years old that at a cost of £843 plus VAT. |
| T = staff costs | £264 | Assume 3 hourly visits with an OT and SLT. The PSSRU 2015 report costs of £44 per hour for a Community OT or SLT. |
| S = resale value | £0 | Assumption |
| r = discount (interest) rate | 3.5% | NICE reference case |
| n = equipment lifespan | 7 years | Assumption |
| A(n,r) = annuity factor (n years at interest rate r) | 6.33 | Calculated |
| Equivalent annual cost | £633 (£500) | Calculated, with refurbishment package (without refurbishment package) |
| Annual maintenance cost | £44 | Annual hourly review with a SLT. The PSSRU 2015 reports a cost of £44 per hour for a Community SLT. |
| Total annual cost | £677 (£544) | Calculated with refurbishment package (without refurbishment package) |
NE-GCE, Electric Programmable Neater Eater; OT, occupational therapist; PSSRU, Personal Social Service Research Unit; SLT, speech and language therapist; VAT, value added tax
As can be seen from Table 3 electro/mechanical assistive devices have an annual cost per person of approximately £677; driven by the high upfront capital cost.
G.3.3.2. Oral motor devices
One trial (Gisel 2001) included in the clinical evidence review evaluated the Innsbruck Sensiromotor Activator and Regulator (ISMAR). The Committee noted that this is one specific type of oral-motor device and the equivalent in the UK would be a palatal training aid (PTA). Similarly to electro/mechanical assistive devices each child or young person with cerebral palsy would receive their own personalised oral-motor device following a successful assessment, but the upfront cost of a PTA would relatively cheap, costing approximately £50 - the total cost of using oral motor devices would be driven by frequent health care professional contact. However, the Committee stated that their use is not wide spread in the UK and is highly dependent on specialist expertise in assessing, manufacturing, fitting and review.
According to the Committee oral motor devices would be made and fitted by an orthodontist and SLT over several visits to the clinic and reviewed, ideally, every 4 months by an orthodontist and SLT to check the fit and functional impact. This would incur an annual maintenance cost of approximately £99 assuming each consultation lasts 15 minutes (Personal Social Service Research Unit [PSSRU] 2015: community SLT per hour, £44; dental services per hour, £88).
Unlike electro/mechanical devices that are used over a person’s lifetime, some children and young people with cerebral palsy abandon oral-motor devices quite quickly if they are uncomfortable, or not effective, whereas others may use for them for several years. As a result the cost-effectiveness of oral motor devices will depend largely on patient preference.
G.3.3.3. Oral sensorimotor treatment
Beckman was one specific exercise programme identified in the clinical evidence review, but the Committee did not consider it was commonly used in the UK. Instead they advised that eating, drinking and swallowing regimens are often developed individually by dysphagia trained SLTs for children and young people with cerebral palsy to perform at their home or school. This would require at least 1 initial visit with a SLT to teach the child or young person with cerebral palsy and their families or carers on how to perform the techniques. Thereafter the SLT would make follow-up visits every 4 to 6 months to assess the impact and modify the treatment programme as necessary. According to the PSSRU 2015 each 30 minute visit with a Community SLT would cost approximately £22.
The duration and frequency of therapeutic interventions, included in the clinical evidence review varied, from over 30 minutes, 5 days per week (Clawson 2007; Ottenbacher 1981), to 1 hour per week (Sigan 2013). In light of this, the Committee noted that families could potentially struggle in day to day practice to follow the intensive regimens applied in some of the research trials; the most families could be expected to achieve is 30 minutes per day, but 3 days per week would be more realistic. Schools may also be able to perform the exercises, but this would require significant staff training if the care staff did not possess the necessary competencies.
The Committee advised that in UK clinical practice oral sensorimotor exercises are undertaken for less than 1 year, depending on the child or young person’s response. Therefore, if the benefits from oral sensorimotor exercises can be achieved in 1 year and maintained over a person’s lifetime without further treatment, oral sensorimotor exercises could be considered cost-effective compared to lifetime management that requires ongoing resources.
G.3.4. Conclusions
The Committee advised that children and young people with cerebral palsy undergo an initial assessment in clinical practice to ensure the benefits of high tech electro/mechanical assistive devices and oral motor devices justify the costs. However, the clinical evidence review found no clinically significant difference in feeding competency between ISMAR devices and no ISMAR devices, questioning if the benefits from ISMAR devices justify the costs for this indication.
On the other hand, a clinically significant benefit was demonstrated for oral sensorimotor treatment versus routine treatment in physical function of the oropharyngeal mechanism. Moreover, oral sensorimotor treatment can be performed at home after 1 initial visit with a SLT; hence the cost of recommending oral sensorimotor treatment would be negligible compared to electro/mechanical assistive devices that are driven by a high upfront capital cost and ongoing health care professional contact.
It is important to note electro/mechanical devices and oral-motor devices do not take time away from a child or young person’s daily activities. Hence, it is important to consider the opportunity cost of their time when performing oral sensorimotor treatment – this treatment may be free to deliver at home, but this does not necessarily mean the exercises should be performed if their quality of life is not improved.
The Committee discussion regarding the associated economic benefits and harms are reported in Section 13.6.3 ‘Evidence to recommendations’
G.4. Optimising nutritional status
G.4.1. Literature review
No economic evaluations of interventions to optimise nutritional status were identified in the literature search conducted for this guideline.
G.4.2. Background and methods
This review question was not prioritised for de novo economic modelling. However, the interventions under consideration vary in the resources and costs required, for example lifestyle changes would be implemented at home by the family or carer, whereas tube feeding would be considerably more expensive. To aid considerations of cost-effectiveness, relevant resource and cost use data are presented.
G.4.3. Resource and cost use
G.4.3.1. Tube feeding
Tube feeding can be used as an adjunct to oral feeding, or if there is clinical concern about the safety of swallowing they can replace oral feeding. Long term interventions to optimise nutritional status include gastrostomy or jejunosotomy tube feeding, whereas nasogastric tube feeding would be used on a shorter term basis. The former are surgical procedures associated with a high cost, whereas the latter can be performed by a nurse as an outpatient procedure. However there are specific clinical implications for long term naso-gastric tube placement that mean they are not the preferred route of enteral feeding beyond short term use.
The costs associated with long-term nutritional supplementation via gastrostomy or nasogastric tube feeding, are outside the scope of NHS Reference Costs and should remain within primary medical services (Department of Health, Reference Costs Guidance 2014-15). For this reason, currency codes related to endoscopic insertions from NHS Reference Costs are presented in Table 4 as a proxy. With regards to nasogastric tube feeding, costs were reported solely for babies under special care (HRG XA03Z); these were considered irrelevant to this review and are not reported.
Table 4Cost of tube feeding procedure
| Procedure | Cost | Source |
|---|---|---|
| Endoscopic Insertion of, Gastrojejunostomy or Jejunostomy Tube, elective inpatient | £1,186 | NHS Reference Costs 2014/15, FZ94Z |
| Endoscopic Insertion of, Gastrojejunostomy or Jejunostomy Tube, day case | £648 | NHS Reference Costs 2014/15, FZ94Z |
| Endoscopic Insertion of Gastrostomy Tube, 18 years and under, elective inpatient | £2,104 | NHS Reference Costs 2014/15, FZ93B |
| Endoscopic Insertion of Gastrostomy Tube, 18 years and under, day case | £1,108 | NHS Reference Costs 2014/15, FZ93B |
The randomised study by Corry 2008 was identified as a relevant source of costing data on tube feeding through ad-hoc searches. This study was included in the Cochrane review on tube feeding for adults with swallowing disturbances. However, it is important to note that Corry 2008 was based on patients with head and neck cancer who required enteral feeding, whose costs may not be generalisable to children and young people with cerebral palsy. They stated that the insertion costs are significantly different as nasogastric tubes are inserted by nursing staff as an outpatient attendance (including the cost of chest X-ray) whereas percutaneous endoscopic gastrostomy tubes are inserted by surgeons in theatre. Table 5 below reports the costs by Corry 2008 alongside inflated sterling prices calculated by the Technical Team.
Table 5Tube feeding resource and cost use reported by Corry 2008
| Resource | NGT | PEG |
|---|---|---|
| Feeding tube cost, 2008 prices | $26 | $110 |
| Insertion costs, 2008 prices | $50 | $626 |
| Total cost of procedure, 2008 prices | $76 | $736 |
| Total cost of procedure, sterlinga | £52 | £503 |
| Total cost of procedure, 2014 pricesb | £59 | £574 |
NGT, nasogastric tube; PEG, percutaneous endoscopic gastrostomy
- a
- b
Inflator to 2015 prices 1.1405, based on the hospital & community health services (HCHS) index (293.1 [2015 PPI] / 257 [2008 PPI])
In addition to the procedure, the Committee advised that some children and young people with cerebral palsy would undergo an intense monitoring schedule during the first few days or weeks with a paediatric nurse specialist. Thereafter the child or young person with cerebral palsy would be monitored on a similar frequency to those receiving high calorie feeds or antimetics, with gastrostomy or jejunosotomy incurring 1 additional visit with their paediatric surgeon each year at a cost of approximately £202 (NHS Reference Costs 2014/15, WF01A, Consultant led Non-Admitted Face to Face Attendance, Follow-up, Paediatric Gastroenterology).
In addition to the monetary cost of tube feeding, the Committee advised that some qualitative reviews show tube feeding can negatively impact a person’s quality of life by affecting social interactions at meal times. Moreover, if the procedure and use of tube feeding is associated with adverse effects, they can incur further treatment costs and decrements in quality of life.
The Committee highlighted that nasogastric tubes frequently fall out and require the cost of a health care professional to reapply to tube if the family/carer were unable to do so. The Committee also added that there are a number of clinical concerns to their long term usage. Equally gastrostomy and jejunostomy tubes, need routine and on occasion emergency replacement which on occasion need professional rather than parent intervention. It was also noted that tube feeding, when used appropriately, positively impacts on clinical wellbeing and health, improving quality of life, justifying the high costs tube feeding can entail in those cases.
G.4.3.2. High calorie feeds
The Committee highlighted 2 commonly used high calorie supplements used to optimise nutrition in children and young people with cerebral palsy: Calogen® and Maxijul®; the cost of these supplements are reported in Table 6.
Table 6Cost of high calorie supplements
| High calorie supplement | Quantity | Pricea |
|---|---|---|
| Calogen®b | 200ml | £4.36 |
| Calogen®b | 500ml | £10.72 |
| Maxijul® Super Soluble | 200g | £2.60 |
| Maxijul® Super Soluble | 528g | £6.48 |
| Maxijul® Super Soluble | 25,000g | £155.56 |
- a
taken from the BNF (NHS indicative price, October (2016)
- b
banana, neutral or strawberry emulsion
Ultimately the cost of high calorie feeds will depend on the frequency those feeds are administered. If those feeds were used to substitute rather than complement diet at home, the cost could be substantial. However, the person’s diet would be reviewed and modified prior to consideration of high calorie feeds, hence the health care professional should determine the appropriate frequency of high calorie supplements.
G.4.3.3. Antimetics
Table 7 presents the acquisition cost of antiemetic drugs, over 1 day and 1 month of continued use, according to the cost reported in the October 2016 NHS Electronic Drug Tariff. For this cost description, BNF dosages were the preferred costing method because trial dosages may not reflect UK clinical practice. Moreover, not all interventions have been identified in the clinical evidence review.
For domperidone and metoclopramide the BNF reports a range of doses to prevent nausea and vomiting according to age and weight. To represent the range of conceivable costs Table 7 presents costs for the maximum dose and a midpoint. The full range of preparations is also reported to demonstrate the variability of costs within each drug.
Erythromcin was also considered by the Committee to be used as an antiemetic/pro-motility in low doses (125mg twice daily); however this would be used off-license to prevent nausea and vomiting.
It is evident from Table 7 that oral solutions of domperidone and metoclopramide are substantially more expensive than tablets that cost less than £3 per month. Therefore, when tablets can be tolerated they should be offered instead of oral solutions because they are cheaper and there is no evidence to suggest they are any less effective. If an oral solution is required erythromycin would the cheapest antiemetic at a cost of approximately £10 per month.
Table 7Acquisition cost of antiemetics
| Antiemetics (quantity, basic price) | Unit cost | Cost per day | Cost per month | ||
|---|---|---|---|---|---|
| Domperidonea | 20mg/day | Max. 30mg/day | 20mg/day | Max. 30mg/day | |
| 10mg tablets (30, £0.87) | £0.03 | £0.06 | £0.09 | £1.76 | £2.64 |
| 5mg/5ml oral suspension sugar free (200ml, £13.43) | £0.34/5ml | £1.34 | £2.01 | £40.83 | £61.24 |
| Metoclopramideb | 6mg tds. | Max. 10mg tds. | 6mg tds. | Max. 10mg tds. | |
| 10mg tablets (28, £0.74) | £0.03 | £0.05 | £0.08 | £1.45 | £2.41 |
| 5mg/5ml oral solution sugar free (150ml, £19.77) | £0.66/5ml | £2.37c | £3.95 | £72.12 | £120.20 |
| Erythromycind | 125mg bd. | 125mg bd. | |||
| Erythromycin 250mg gastro-resistant capsules (28, £5.61) | £0.20 | £0.20 | £6.09 | ||
| Erythromycin 250mg gastro-resistant tablets (28, £1.33) | £0.05 | £0.05 | £1.44 | ||
| Erythromycin ethyl succinate 125mg/5ml oral suspension (100ml, £4.05) | £0.20/5ml | £0.41 | £12.31 | ||
| Erythromycin ethyl succinate 125mg/5ml oral suspension sugar free (100ml, £3.58) | £0.18/5ml | £0.36 | £10.88 | ||
| Erythromycin ethyl succinate 250mg/5ml oral suspension (100ml, £6.38) | £0.31/5ml | £0.32 | £9.70 | ||
| Erythromycin ethyl succinate 250mg/5ml oral suspension sugar free (100ml, £5.27) | £0.26/5ml | £0.26 | £8.01 | ||
| Erythromycin stearate 250mg tablets (100, £18.20) | £0.18 | £0.18 | £5.53 | ||
bd, twice daily; tds, 3 times daily
- a
BNF reports the following dosages of domperidone for relief of nausea and vomiting:
Child (body-weight <35 kg): 250 micrograms/kg up to 3 times a day; maximum 750 micrograms/kg per day
Child 12-17 years (body-weight ≥35 kg):10 mg up to 3 times a day; maximum 30 mg per day
Adult (body-weight ≥35 kg): 10 mg up to 3 times a day; maximum 30 mg per day
- b
BNF reports the following dose of metoclopramide for prevention of delayed chemotherapy-induced nausea and vomiting: 100-150 micrograms/kg up to 3 times a day (max. per dose 10 mg)
- c
3.6x 5ml
- d
Can be used as an antiemetic/pro-motility if low doses are given according to the Committee
G.4.4. Conclusions
The clinical evidence review did not produce any evidence and recommendations that would represent a change in current practice, so the least invasive and cheapest options will be implemented first and tube feeding only when clinically appropriate.
Moreover, nutritional issues can range from malnutrition to overweight/obesity; hence interventions would be individualised to the person’s needs.
The Committee’s discussion regarding the associated economic benefits and harms are reported in the Section 14.6.3 ‘Evidence to recommendations’.
G.5. Management of pain, distress and discomfort
G.5.1. Literature review
No economic evaluations of interventions to manage pain, discomfort and distress were identified in the literature search conducted for this guideline.
G.5.2. Background and methods
The evidence base for the clinical evidence reviews did not identify any relevant studies to show which interventions are clinically effective in reducing pain and distress in children and young people with cerebral palsy. Despite this, it is important to consider that the interventions included in this review differ in their resources and costs. For example, some non-pharmacological treatments require weekly sessions with a health care professional, whereas others could be performed at home by the family or carer.
The Committee also highlighted that provision across the country is variable, with some health care professionals reluctant to prescribe pharmacological treatments. For these reasons, relevant resource and cost use data are presented to aid consideration of cost-effectiveness.
G.5.3. Resource and cost use
Pharmacological treatments are presented over 1 day and a typical monthly cost of continued use in Section G.5.3.1. When a range of doses is reported according to age, severity and/or weight the mid-point or range is presented to represent the full scope of costs. In addition, all appropriate preparations are reported to demonstrate the variability of costs within each drug.
Drug acquisition costs are taken from the October 2016 NHS Electronic Drug Tariff, unless otherwise stated. Dosages of certain drugs used outside their normal area of action reflect those reported by the Committee as the BNF often reported indications and doses that related to epilepsy, seizures, convulsions or bipolar disorder which are not necessarily the primary reason for their use in children and young people with cerebral palsy, particularly if the drugs are prescribed to reduce pain and distress.
General practitioners (GPs) often refer children and young people with cerebral palsy to their specialist centre when pharmacological treatments for pain or distress are required. Ideally, children and young people with cerebral palsy would be reviewed at least every 3 months by their specialist centre. According to NHS Reference Costs 2014/15 the national average cost for a consultant led (non-admitted) follow-up paediatric pain management attendance is £561.
For non-pharmacological treatments, the frequency of administration and monitoring would depend on the potential causes of pain, and this may be conducted outside of the specialist centre. Typical resource and cost use associated with psychological therapy, physical therapy and hydrotherapy are outlined in Section G.5.3.2.
G.5.3.1. Pharmacological
Analgesics
The Committee provided the following dosages of paracetamol according to age, but also stated that the dose would depend on the severity of pain:
- 3 to 12 months, 60 to 120mg every 4 to 6 hours;
- 1 to 5 years, 120 to 240mg every 4 to 6 hours;
- 6 to 12 years, 250 to 500mg every 4 to 6 hours;
- 12 to 18 years, 500mg to 1g every 4 to 6 hours.
Table 8 below presents the cost of all appropriate preparations of paracetamol over the course of 1 day and 1 month: 120mg 3 times a day and 500mg 3 times a day; chosen to illustrate those ranges above.
Similarly to paracetamol, the dose of ibuprofen depends on age and severity; ranging from 50mg 3 times a day to 300mg 3 times a day. Table 8 below presents the acquisition cost of ibuprofen at either end of this range to reflect the range of conceivable costs.
It is evident from Table 8 that oral solutions, orodispersible tablets and chewable capsules (ibuprofen) are the most expensive preparations of analgesics. Conversely, capsules and tablets are relatively cheap, with a negligible difference in cost between paracetamol and ibuprofen. Therefore, when capsules or tablets can be tolerated, they should be offered instead of oral solutions because they are cheaper and there is no evidence to suggest they are any less effective.
Table 8Acquisition cost of analgesics
| Analgesic(quantity, basic price) | Unit cost | Cost per day | Cost per month | ||
|---|---|---|---|---|---|
| Paracetamol | 120mg tds | 500mg tds | 120mg tds | 500mg tds | |
| 120mg/5ml oral solution paediatric sugar free (500ml, £2.86) | £0.03/5ml | £0.09 | £0.36a | £2.61 | £10.87 |
| 500mg/5ml oral solution sugar free (150ml, £18.00) | £0.60/5ml | £0.43b | £1.80 | £13.13 | £54.72 |
| 500mg capsules (32, £0.91) | £0.03 | NA | £0.09 | NA | £2.59 |
| 500mg capsules (100, £2.84) | £0.03 | NA | £0.09 | NA | £2.59 |
| 500mg tablets (32, £0.73) | £0.03 | £0.03c | £0.09 | £0.87 | £2.62 |
| 500mg tablets (100, £2.28) | £0.03 | £0.03c | £0.09 | £0.88 | £2.63 |
| 250mg orodispersible tablets (12, £2.28, BNF) | £0.19 | £0.38d | £1.14 | £11.55 | £34.66 |
| 250mgorodispersible tablets (24, £3.59, BNF) | £0.15 | £0.30d | £0.90 | £9.09 | £27.28 |
| Ibuprofen | 50mg tds | 300mg tds | 50mg tds | 300mg tds | |
| 200mg tablets (24, £0.97) | £0.04 | £0.04c | £0.18e | £1.23 | £5.53 |
| 200mg tablets (84, £3.40) | £0.04 | £0.04c | £0.18e | £1.23 | £5.54 |
| 400mg tablets (24, £0.89) | £0.04 | NA | £0.09f | NA | £2.87 |
| 400mg tablets (84, £3.12) | £0.04 | NA | £0.09f | NA | £2.87 |
| 600mg tablets (84, £5.77) | £0.07 | NA | £0.10g | NA | £3.13 |
| 100mg/5ml oral suspension sugar free (100ml, £1.33) | £0.07/5ml | £0.10h | £0.60i | £3.03 | £18.19 |
| 600mg effervescent granules (20, £6.80, BNF) | £0.34 | NA | £0.51 | NA | £15.50 |
| 100mg chewable capsules (12, £3.23, BNF) | £0.27 | £0.40 | £2.42 | £12.27 | £73.64 |
| 200mg orodispersible tablets (12, £2.00) | £0.17 | £0.17c | £0.83e | £5.07 | £25.33 |
| 200mg capsules (30, £4.40) | £0.15 | NA | £0.73e | NA | £22.29 |
tds, 3 times daily
- a
12.5x 5ml
- b
0.72x 5ml
- c
1 tablet or capsule per day (assuming no carry over)
- d
2 tablets per day (assuming no carry over)
- e
4.5x 1 200mg tablet or capsule
- f
2x 1 400mg table plus 0.5x 1 200mg tablet
- g
1.5x 1 600mg tablet
- h
1.5x 5ml
- i
9x 5ml
Anticonvulsants
Some anticonvulsant agents are also used for pain relief, especially for neuropathic pain. In particular gabapentin, pregabalin and carbamazepine have a recognised role in management of acute and chronic pain, with sodium valproate less so.
For carbamazepine, the Committee advised an initial dose of 2.5mg/kg twice daily increasing to 5mg/kg twice daily as necessary, for gabapentin 5mg/kg up to a maximum of 300mg 3 times a day and for sodium valproate a range from 20mg/kg a day to 30mg/kg a day.
Costs increase in proportion with weight up to any maximum dose, but for illustrative purposes, 2 doses are costed to represent children and young people weighing approximately 30kg and 50kg. In Table 9 only the initial dose of carbamazepine (2.5mg/kg) has been costed, but the increased dose (5mg/kg) can be estimated by doubling.
Similarly to analgesics (Section0) Table 9 shows that oral solutions (particularly gabapentin 500mg/ml oral suspension sugar free) are the most expensive preparations. Conversely, capsules and tablets are relatively cheap, with a negligible difference in the cost between the cheapest preparations of gabapentin (capsules), carbamazepine (tablets) and sodium valproate (gastro-resistant tablets).
Table 9Acquisition cost of anticonvulsants
| Anticonvulsant (quantity, basic price) | Unit cost | Cost per day | Cost per month | ||
|---|---|---|---|---|---|
| 30kg | 50kg | 30kg | 50kg | ||
| Gabapentin | 150mg tds | 250mg tds | 150mg tds | 250mg tds | |
| 600mg tablets (100, £8.50) | £0.09 | £0.06a | £0.11e | £1.94 | £3.23 |
| 800mg tablets (100, £28.47) | £0.28 | NA | £0.28f | NA | £8.65 |
| 100mg capsules (100, £2.00) | £0.02 | £0.09b | £0.15g | £2.74 | £4.56 |
| 300mg capsules (100, £2.91) | £0.03 | £0.04c | £0.07h | £1.33 | £2.21 |
| 400mg capsules (100, £4.44) | £0.04 | NA | £0.09i | NA | £2.70 |
| 50mg/ml oral solution sugar free (150ml, £69.00) | £0.46/ml | £4.14d | £6.90j | £125.86 | £209.76 |
| Carbamazepine | 75mg bd | 125mg bd | 75mg bd | 125mg bd | |
| 100mg tablets (84, 2.07) | £0.02 | £0.04k | £0.06m | £1.12 | £1.87 |
| 200mg tablets (84, £3.83) | £0.05 | £0.21f | £0.22n | £6.33 | £6.70 |
| 400mg tablets (56, £5.02) | £0.09 | NA | NA | NA | NA |
| 400mg modified-release tablets (56, £10.24) | £0.18 | NA | NA | NA | NA |
| 200mg modified-release tablets (56, £5.20) | £0.09 | NA | £0.12n | NA | £3.53 |
| 100mg/5ml oral suspension sugar free (300ml, £6.12) | £0.10/5ml | £0.08l | £0.26o | £2.33 | £7.75 |
| Sodium valproate | 800mg day | 1.2g day | 800mg day | 1.2g day | |
| 100mg tablets (100, £5.60) | £0.06 | £0.45 | £0.67 | £13.62 | £20.43 |
| 200mg gastro-resistant tablets (100, £4.75) | £0.05 | £0.19 | £0.29 | £5.78 | £8.66 |
| 200mg/5ml oral solution (300ml, £9.33) | £0.16/5ml | £0.62 | £0.93 | £18.91 | £28.36 |
| 200mg/5ml oral solution sugar free (300ml, £5.01) | £0.09/5ml | £0.33 | £0.50 | £10.15 | £15.23 |
| 200mg gastro-resistant tablets (100, £4.75) | £0.05 | £0.18 | £0.28 | £5.61 | £8.41 |
| 300mg modified release capsules (100, £13.00) | £0.13 | £0.39r | £0.52 | £11.86 | £15.81 |
| 300mg modified release tablets (100, £17.47) | £0.12 | £0.36r | £0.49 | £11.06 | £14.75 |
| 500mg gastro-resistant tablets (100, £8.72) | £0.09 | £0.17p | £0.22q | £5.30 | £6.75 |
| 500mg modified release granule sachets (100, £21.00) | £0.21 | £1.21s | £1.42t | £36.78 | £43.17 |
| 500mg modified-release tablets (100, £29.10) | £0.29 | £0.65u | £1.07v | £19.91 | £32.44 |
bd, twice daily; tds, 3 times daily
- a
0.75x 1 600mg tablet
- b
4.5x 1 100mg capsule
- c
1.5x 1 300mg capsule
- d
9ml
- e
1.25x 1 600mg tablet
- f
1 tablet
- g
7.5x 1 100mg capsule
- h
2.5x 1 300mg capsule
- i
2x 1 400mg capsule
- j
5ml
- k
5x 1 100mg tablet
- l
0.75x 5ml
- m
2.5x 1 100mg tablet
- n
1 200mg tablet plus half 100mg tablet
- o
2.5x 5ml
- p
2 tablets per day (assuming no carry over)
- q
2 500mg tablets plus 1 200mg tablet
- r
3 tablets per day (assuming no carry over)
- s
1 500mg sachet plus 1 300mg sachet
- t
2 500mg sachets plus 1 300mg sachets
- u
1 500mg modified release tablet plus 1 300mg modified release tablet
- v
2 500mg modified release tablet plus 1 300mg modified release tablet
Pregabalin
The Committee stated that the dose of pregabalin received by children and young people with cerebral palsy depends on age and severity; ranging from 150mg a day to 300mg a day. Table 10 below presents the acquisition cost of pregabalin across 1 day and 1 month at either end of this range to reflect the range of conceivable costs.
Table 10Acquisition cost of pregabalin
| Pregabalin (quantity, basic price) | Unit cost | Cost per day | Cost per month | ||
|---|---|---|---|---|---|
| 150mg day | 300mg day | 150mg day | 300mg day | ||
| 25mg capsules (56, £64.40) | £1.15 | NA | NA | NA | NA |
| 50mg capsules (84, £96.60) | £1.15 | NA | NA | NA | NA |
| 75mg capsules (56, £64.40) | £1.15 | NA | NA | NA | NA |
| 100mg capsules (84, £96.60) | £1.15 | NA | NA | NA | NA |
| 150mg capsules (56, £64.40) | £1.15 | £1.15 | NA | £34.96 | NA |
| 200mg capsules (84, £96.60) | £1.15 | NA | NA | NA | NA |
| 225mg capsules (56, £64.40) | £1.15 | NA | NA | NA | NA |
| 300mg capsules (56, £64.40) | £1.15 | NA | £1.15 | NA | £34.96 |
| 20mg/ml oral solution sugar free (473ml, £84.56) | £0.18/ml | £1.34a | £2.68b | £40.76 | £81.52 |
- a
7.5ml
- b
15ml
It is evident from Table 10 that the unit cost of pregabalin capsules do not vary with concentration. Conversely, the cost of oral solution increases as the dose increases. When comparing pregabalin to the anticonvulsants reported in Table 9, it can be seen that pregabalin is the most expensive anticonvulsant.
Benzodiazepines: diazepam
The Committee stated that diazepam is usually prescribed 0.25mg/kg twice daily, but could also be stratified into the following ages for children and young people with cerebral palsy:
- 1 to 4 years, 2.5mg twice daily;
- 5 to 12 years, 5mg twice daily;
- Over 13 years, 10mg twice daily.
Based on those ages, Table 11 below presents the cost of diazepam over the course of 1 day and 1 month.
Table 11Acquisition cost of diazepam
| Diazepam (quantity, basic price) | Unit cost | Cost per day | Cost per month | ||||
|---|---|---|---|---|---|---|---|
| 1 to 4 years | 5 to 12 years | ≥13 years | 1 to 4 years | 5 to 12 years | ≥13 years | ||
| 2mg tablet (28, £0.75) | £0.03 | £0.07a | NA | NA | £2.04 | NA | NA |
| 5mg tablet (28, £0.78) | £0.03 | £0.03b | £0.06 | NA | £0.85 | £1.69 | NA |
| 10mg tablet (28, £0.93) | £0.03 | NA | £0.03c | £0.07 | NA | £1.01 | £2.02 |
| 2mg/5ml oral solution sugar free (100ml, £31.75) | £1.59/5ml | £3.97d | £7.94e | £15.88f | £120.65 | £241.30 | £482.60 |
- a
2.5x 2mg tablet
- b
1 5mg tablet split in half for each dose
- c
1 10mg tablet split in half for each dose
- d
2.5x 5ml
- e
5x 5ml
- f
10x 5ml
It is evident from Table 11 that oral solution is substantially more expensive than tablets. Moreover, diazepam oral solution is the most expensive oral solution under consideration. However, the tablet preparation of diazepam is one of the cheapest interventions under consideration, demonstrating that the preparation of a drug has a large impact on cost.
Opioids: Fentanyl patches
The Committee advised that children and young people with cerebral palsy who require a fentanyl patch should be under the care of a specialist pain team in tertiary care. Ideally a pain specialist would supervise a child on a patch, but this would be less common in adult services. According to NHS Reference Costs 2014/15 the national average cost for a consultant led (non-admitted) follow-up paediatric pain management attendance is £561. Table 12 below presents the acquisition cost of fentanyl transdermal patches; these would be used continuously for 3 days, repeated as necessary.
Table 12Acquisition cost of fentanyl patches
| Fentanyl patches (quantity, basic price) | Unit cost |
|---|---|
| 12micrograms/hour transdermal patches (5, £12.59) | £2.52 |
| 25micrograms/hour transdermal patches (5, £17.99) | £3.60 |
| 50micrograms/hour transdermal patches (5, £33.66) | £6.73 |
| 75micrograms/hour transdermal patches (5, £46.99) | £9.40 |
| 100micrograms/hour transdermal patches (5, £57.86) | £11.57 |
G.5.3.2. Non-pharmacological
Psychological therapy
The Committee advised that interventions such as cognitive behavioural therapy (CBT) would need to be performed with a psychologist (banding 8a or above), intensively on a weekly basis for 10 weeks, with further follow up sessions as required. According to the PSSRU 2015 the cost for a 55 minute CBT session based on staff earnings for a speciality doctor (midpoint), clinical psychologist (band 8 median) and mental health nurse (band 6 median) is £98, leading to an initial cost of £980 if 10 sessions are required.
Due to the difficulties of accessing these service promptly on the NHS, teaching psychological strategies to families or carers to support the children and young people with cerebral palsy after the course of intensive health care professional input would be advantageous. However, the Committee noted that not all families or carers could engage with this.
Physical therapy
The Committee advised that physical therapy such as heat, exercise, massage, or ultrasound therapy would require high intensity short sessions of treatment of a similar duration to psychological therapy.
Physical exercise programmes to reduce pain would be tailored to each child or young person with cerebral palsy by physiotherapists. Initially the program would be performed with a physiotherapist to teach the family or carer the techniques. These techniques could then be replicated at home at no monetary cost if the family or carer possessed the necessary competencies. Health care professional advice would then be sought if there was a change in function, or family or carer concern.
According to NHS Reference Costs 2014/15 the national average cost for a non-consultant led (non-admitted) follow-up occupational therapy attendance is £67, and the cost for a non-consultant led (non-admitted) follow-up physiotherapy attendance is £42.
Heat therapy would usually be part of a home management plan performed at home by the carer or family once deemed appropriate and safe. Conversely, massage and ultrasound therapy would require a health care professional to deliver the intervention successfully. For ultrasound therapy provided by a pain management service as an outpatient procedure, NHS Reference Costs 2014/15 report a cost of £145 (currency code, MA36Z; service code, 191).
Hydrotherapy
The Committee advised that hydrotherapy sessions should be led by a physiotherapist when the aim is to reduce pain. NHS Reference Costs 2014/15 report a national average cost of £42 for a non-consultant led (non-admitted) follow-up physiotherapy attendance.
G.5.4. Conclusions
Pharmacological treatments prescribed as a capsule or tablet preparation are relatively inexpensive compared to oral solutions. Therefore, when capsules or tablets can be tolerated they should be offered instead of oral solutions as there is no evidence to suggest they are any less effective.
Psychological therapy entails a high upfront cost, but over the longer term family members or carers could learn the techniques which could reduce future health care professional involvement. Conversely, hydrotherapy and some physical therapies would require health care professional supervision when they are performed to reduce pain to ensure the pain is targeted correctly. Therefore those interventions that incur additional resources will need to provide additional benefits in relation to their cheaper comparators to be considered cost-effective.
Overall, in the absence of data on effectiveness the cost-effectiveness of these interventions cannot be ascertained.
The Committee’s discussion regarding the associated economic benefits and harms are reported in Section 22.5.3 ‘Evidence to recommendations’.
G.6. Managing sleep disturbance in children and young people with cerebral palsy
G.6.1. Literature review
No economic evaluations of interventions to manage sleep disturbances were identified in the literature search conducted for this guideline.
G.6.2. Background and methods
This review question was not prioritised for de novo economic modelling. However the interventions under consideration have different resources implications. For example modifying sleep routine or positioning could be performed at home without a health care professional, whereas pharmacological treatments incur acquisition costs. The Committee has also highlighted that current practice is varied. Therefore, relevant resource and cost use data are presented to aid considerations of cost-effectiveness.
G.6.3. Resource and cost use
A daily and typical monthly cost based on continued use are presented for pharmacological treatments in Sections G.6.3.1 and G.6.3.2. When a range of doses is reported according to age and/or weight the mid-point or range is presented to represent the full scope of costs.
Moreover, all appropriate preparations are reported to demonstrate the variability of costs within each drug.
Drug acquisition costs are taken from October 2016 NHS Electronic Drug Tariff. For this cost description, dosages informed by the BNF, or the Committee, were the preferred costing method because trial dosages may not reflect UK clinical practice. Moreover, not all interventions have been identified in the clinical evidence review.
The Committee stated that GPs often refer children and young people with cerebral palsy to their specialist cerebral palsy centre when pharmacological treatments for sleep are required. Ideally they would be reviewed at least every 3 months by their specialist centre.
Non-pharmacological treatments can include sleep systems or modifications to the person’s sleep routine. The former would incur an upfront capital cost and equipment review costs, whereas the latter programme would be relatively cheap as it is managed in the home by the parents and carers. Typical resource and cost use data associated with sleep systems are outlined in Section G.6.3.3.
G.6.3.1. Melatonin
Melatonin is available as a modified-release tablet (Circadin®) and also as unlicensed formulations. Circadin® is licensed for the short-term treatment of primary insomnia in adults over 55 years, but unlicensed immediate-release preparations are available. The BNF reports the following dose for sleep onset insomnia and delayed sleep phase syndrome in children aged 1 month to 18 years:
- initially 2 to 3 mg daily before bedtime;
- increased if necessary after 1 to 2 weeks to 4 to 6 mg daily before bedtime;
- max. 10 mg daily.
Similarly the Committee advised the following dosages for children and young people with cerebral palsy stratified by age:
- 2 to 3mg daily in children under 5;
- 6mg daily in children over 5;
- max. 12mg daily.
Table 13 below presents the acquisition cost of Circadin® across 1 day and 1 month for 3 dosages (3mg, 6mg and 10mg) to reflect a range of conceivable costs. However, other formulations of melatonin are available from ‘special-order’ manufacturers, or specialist importing companies.
Table 13Acquisition cost of melatonin
| Melatonin (quantity, basic price) | Unit cost | Cost per day | Cost per month | ||||
|---|---|---|---|---|---|---|---|
| 3mg daily | 6mg daily | 10mg daily | 3mg daily | 6mg daily | 10mg daily | ||
| Circadin® 2mg (30, £15.39) | £0.51 | £0.77 | £1.54 | £2.57 | £23.39 | £46.79 | £77.98 |
G.6.3.2. Sedatives
Alimemazine
Alimemazine is licensed as a sedative for children aged between 2 and 7 years and the BNF recommends a dose of up to max. 2 mg/kg 1 to 2 hours before their operation. However, the Committee stated that a dose of 1mg/kg up to a maximum of 60mg would be more appropriate to reduce sleep disturbance in children and young people with cerebral palsy.
Table 14 below presents the acquisition cost of alimemazine for 1 day and for 1 month based on the dose suggested by the Committee. For illustrative purposes, costs are presented for children with a weight of 30kg and 50kg but costs increase in proportion with weight up to a maximum dose of 60mg.
Table 14Acquisition cost of alimemazine
| Alimemazine (quantity, basic price) | Unit cost | Cost per day | Cost per month | ||
|---|---|---|---|---|---|
| 30kg (30mg/day) | 50kg (50mg/day) | 30kg (30mg/day) | 50kg (50mg/day) | ||
| 10mg tablets (28, £102.59) | £3.66 | £10.99 | £18.32 | £334.15 | £556.92 |
| 30mg/5ml oral solution (100ml, £221.37) | £11.07/5ml | £11.07 | £18.82a | £336.51 | £572.07 |
| 7.5mg/5ml oral solution (100ml, £163.21) | £8.16/5ml | £32.64b | £54.68c | £992.32 | £1,662.13 |
- a
1.7x 5ml
- b
4x 5ml
- c
6.7x 5ml
Clonidine
The BNF states that clonidine is not licensed for use in children, but would be used off license for sedation in adults. Despite this, the Committee stated that children and young people with cerebral palsy could receive 30 to 50 mcg daily before bedtime to reduce sleep disturbances. Table 15 below presents the acquisition cost of clonidine for 1 day and for 1 month for this range.
Chloral hydrate
Chloral hydrate is an older drug which retains some limited clinical usage. The licensed products in the UK are Welldorm® elixir (containing chloral hydrate) and Welldorm® tablets (containing a precursor, chloral betaine) for the short-term treatment of severe insomnia which is interfering with normal daily life in adults and in children aged 2 years or older.
The BNF recommends the following dosages for Welldorm® elixir to treat insomnia in children:
- child 2 to 11 years 1–1.75 mL/kilogram, alternatively 30–50 mg/kg, dose to be taken with water or milk at bedtime; maximum 35 mL per day; maximum 1 g per day;
- child 12 to 18 years 15–45 mL, alternatively 0.4–1.3 g, dose to be taken with water or milk at bedtime; maximum 70 mL per day; maximum 2 g per day.
Similarly, the Committee advised a dose 30mg/kg daily before bedtime, up to a maximum dose of 2g to reduce sleep disturbances in children and young people with cerebral palsy.
Table 16 below presents the acquisition cost of chloral hydrate for 1 day and for 1 month based on the dose reported by the Committee. For illustrative purposes, costs are presented for children with a weight of 30kg and 50kg but costs increase in proportion with weight up to a maximum dose of 2g.
It should also be noted that other formulations of chloral hydrate are also available from ‘special-order’ manufacturers or specialist importing companies.
Table 16Acquisition cost of chloral hydrate
| Chloral hydrate (quantity, basic price) | Unit cost | Cost per day | Cost per month | ||||
|---|---|---|---|---|---|---|---|
| 30kg (900mg/day) | 50kg (1.5g/day) | >67kg (max. 2g) | 30kg (900mg/day) | 50kg (1.5g/day) | >67kg (max. 2g) | ||
| 143.3mg/5ml oral solution BP (150ml, £244.26) | £8.14/5ml | £51.29a | £85.49b | £113.98c | £1,559.29 | £2,598.82 | £3,465.09 |
- a
6.3x 5ml
- b
10.5x 5ml
- c
14x 5ml
G.6.3.3. Non-pharmacological
There are many different types of sleep systems available such as postural devices, wedges and supports that vary in price according to the manufacture, attachments and size. Based on this, it would be inappropriate to suggest a “one-price-fits-all” because the equipment would be individualised to the child or young person with cerebral palsy; from a list of manufactures and systems provided by the Committee, the upfront capital cost could range from approximately £100 to £1,000.
The Committee also advised that sleep positioning equipment is usually prescribed with room for growth in mind with a lifespan of approximately 3 to 5 years, but this would vary according to the type of sleep system.
With those factors in mind, there are 2 aspects to capital costs:
- Opportunity cost – this is the money spent on equipment that could have been invested in another venture. This cost is calculated by applying an interest rate on the sum invested in the capital.
- Depreciation cost – the equipment has a certain lifespan and depreciates over time, and will eventually need to be replaced.
The usual practice for economic evaluation is to calculate an ‘annual equivalent cost’. This is calculated by annuitizing the initial capital outlay over the expected life of the equipment. Calculating the equivalent annual cost means making allowance for the differential timing of costs by discounting.
Due to the variations in cost and lifespan described, the equivalent annual cost could range from £26 to £263, for capital costs of £100 to £1,000, respectively, over 4 years.
In addition to the initial capital outlay, the equipment should be reviewed annually, especially with children as the set up would need to be adjusted for growth and changes in their presentation. Ideally the equipment would be reviewed annually by the health care professional who issued the equipment (occupational therapists, physiotherapists or social care occupational therapists), but this may be increased in children and young people with more complex needs, or reduced to when a need is identified by the family or carer. Moreover families or carers should be able to contact services if they identify a need between reviews.
The cost per hour of patient contact with a community physiotherapist or community occupational therapist is £44 according to the PSSRU 2015. The cost per hour includes the costs of overheads, but does not take into account the travel time required by community therapists. Based on 2, 1 hour reviews per year (£88) the total cost per year could range from £114 to £351 (for capital costs of £100 to £1,000, respectively, over 4 years).
An initial assessment by familiar therapists and an equipment representative should be carried out with the child or young person with cerebral palsy and their main carers who will be using the equipment. The equipment should then be left with the family for a few days to see how the child or young person responds. As a result, only children and young people with cerebral palsy who are expected to benefit from sleep systems from this assessment would receive one in clinical practice. However, Lloyd 2014 found no significant difference in sleep initiation and maintenance for sleep systems versus no sleep systems which questions if the benefits of sleep systems justify the cost.
G.6.4. Conclusions
Clonidine is the cheapest pharmacological treatment under consideration (regardless of the preparation chosen) whereas choral hydrate oral solution is the most expensive. Consequently, chloral hydrate would need to provide the greatest benefit relative to its comparators to be considered cost-effective. However, in the absence of data on the effectiveness of sedatives, the cost-effectiveness relative to any of the interventions included in this review cannot be ascertained.
In clinical practice, sleep systems are individualised to the child or young person’s needs and in some cases, they can entail a high upfront cost. In clinical practice children and young people with cerebral palsy would undergo an initial assessment to ensure they responded positively to their sleep system to ensure the benefits from sleep systems justify the costs. However, if cost-effectiveness is ascertained from the clinical effectiveness data reported by Lloyd 2014 sleep systems would not be considered cost-effective relative to no sleep systems.
The meta-analysis undertaken by the technical team found melatonin provided a clinically statistically significant improvement in sleep latency compared to placebo, but no clinically statistically significant difference in total night sleep time or night wakes. Therefore, if the Committee believe the benefits from sleep latency can justify the costs, melatonin could be considered cost-effective relative to placebo.
The Committee’s discussion regarding the associated economic benefits and harms are reported in Section 23.6.3 ‘Evidence to recommendations’.
G.7. Managing mental health problems in children and young people with cerebral palsy
G.7.1. Literature review
No economic evaluations of interventions to manage mental health problems were identified in the literature search conducted for this guideline.
G.7.2. Background and methods
This review question was not prioritised for de novo economic modelling. However, the interventions under consideration vary in the resources and costs required; for example the family or carer could implement behavioural techniques at home, whereas regular psychotherapy sessions would incur high staff costs. To aid considerations of cost-effectiveness, relevant resource and cost use data are presented.
G.7.3. Resource and cost use
G.7.3.1. Non-pharmacological
The cost per cognitive behavioural therapy (CBT) and psychotherapy attendance is presented in Table 17.
Table 17Cost of psychotherapy attendances
| Service | National average | Lower quartile | Upper quartile | Source |
|---|---|---|---|---|
| Child and Adolescent Psychiatry | £186 | £79 | £259 | NHS Reference Costs 2014/15, consultant led, service 711, NonAdmitted Face to Face Attendance, Follow-up, WF01A |
| Psychotherapy | £196 | £162 | £213 | NHS Reference Costs 2014/15, consultant led, service 713, NonAdmitted Face to Face Attendance, Follow-up, WF01A |
| CBT | £98 | NR | NR | PSSRU 2015 for a 55 minute session based on staff earnings for a speciality doctor (midpoint), clinical psychologist (band 8 median) and mental health nurse (band 6 median) |
CBT, cognitive behavioural therapy; NR, not reported; PSSRU, Personal Social Services Research Unit
G.7.3.2. Pharmacological: antidepressants & anxiolytics
Pharmacological acquisition costs are presented over the course of 1 day and 1 month of continued use in Table 18 based on the costs reported in the October 2016 NHS Electronic Drug Tariff. For this cost description BNF dosages, unless otherwise stated, were the preferred costing method because trial dosages my not reflect UK clinical practice. Moreover, no pharmacological interventions were identified in the clinical evidence review. Antidepressants and anxiolytics would be administered at home, ideally following an assessment with a specialist psychiatrist (NHS Reference Cost 2015, WF01B, Consultant-led, First Attendance, Non-Admitted Face To Face: Service code 171, Child and Adolescent Psychiatry, £171; Service Code 713, Psychotherapy, £227).
The BNF reports a range of doses; hence, to represent the range of conceivable costs Table 18 presents costs for the maximum dose and an arbitrary midpoint. Appropriate preparations are also reported to demonstrate the variability of costs within each drug.
Table 18Acquisition cost of antidepressants & anxiolytics
| Drug (quantity, basic price) | Unit cost | Cost per day | Cost per month | ||
|---|---|---|---|---|---|
| Diazepama | 500ug bd | Max. 2mg bd | 500ug bd | Max. 2mg bd | |
| Diazepam 2mg tablets (28, £0.75) | £0.03 | £0.03 | £0.05 | £0.91 | £1.63 |
| Diazepam 5mg tablets (28, £0.78) | £0.03 | NA | NA | NA | NA |
| Diazepam 2mg/5ml oral solution sugar free (100ml, £31.75) | £1.59/5ml | £0.79 | £3.18 | £24.13 | £96.52 |
| Fluoxetineb | 10mg/day | Max. 20mg/day | 10mg/day | Max. 20mg/day | |
| Fluoxetine 20mg dispersible tablets (28, £3.44) | £0.12 | £0.12c | £0.12 | £3.73 | £3.73 |
| Fluoxetine 20mg capsules (30, £0.94) | £0.03 | £0.03c | £0.03 | £0.95 | £0.95 |
| Fluoxetine 60mg capsules (30, £8.99) | £0.30 | NA | NA | NA | NA |
| Fluoxetine 20mg/5ml oral solution (70ml, £2.96) | £0.23 | £0.11 | £0.21 | £3.21 | £6.43 |
| Fluoxetine 20mg/5ml oral solution sugar free (70ml, £12.95) | £0.93 | £0.46 | £0.93 | £14.06 | £28.12 |
| Citalopram | Low dosed | Max.e | Low dosed | Max.e | |
| Citalopram 10mg tablets (28, £0.79)f | £0.03 | £0.06 | £0.11 | £1.72 | £3.43 |
| Citalopram 20mg tablets (28, £0.86)f | £0.03 | £0.03 | £0.06 | £0.93 | £1.87 |
| Citalopram 40mg tablets (28, £0.90)f | £0.03 | NA | £0.03 | NA | £0.98 |
| Citalopram 40mg/ml oral drops sugar free (15, £5.04)g | £0.34 | £0.13 | £0.27 | £4.09 | £8.17 |
| Sertralineh,i | 50mg/day | Max. 200mg/day | 50mg/day | Max. 200mg/day | |
| Sertraline 50mg tablets (28, £1.23) | £0.04 | £0.04 | £0.18 | £1.34 | £5.34 |
| Sertraline 100mg tablets (28, £1.38) | £0.05 | NA | £0.10 | NA | £3.00 |
| Amitriptyline j | 75mg/day | Max. 200mg/day | 75mg/day | Max. 200mg/day | |
| Amitriptyline 10mg tablets (28, £1.20) | £0.04 | NA | NA | NA | NA |
| Amitriptyline 25mg tablets (28, £0.79) | £0.03 | £0.08 | NA | £2.57 | NA |
| Amitriptyline 50mg tablets (28, £1.15) | £0.04 | £0.07k | £0.16 | £2.11k | £4.43 |
| Amitriptyline 25mg/5ml oral solution sugar free (150ml, £18.00) | £0.60 | £1.80 | NA | £54.72 | NA |
| Amitriptyline 50mg/5ml oral solution sugar free (150ml, £19.20) | £0.64 | £0.96 | £2.56 | £29.18 | £77.82 |
| Buspironel | 5mg tds | Max. 30mg/day | 5mg tds | Max. 30mg/day | |
| Buspirone 5mg tablets (30, £3.38) | £0.11 | £0.34 | NA | £10.28 | NA |
| Buspirone 10mg tablets (30, £4.20) | £0.14 | NA | £0.42 | NA | £12.77 |
bd, twice daily; tds, 3 times daily; NA, not applicable
- a
BNF dose for anxiety: by mouth; adult, 2 mg 3 times a day, then increased if necessary to 15-30 mg daily in divided doses Costing based on Committee dose for a anxiolytic indication: age 4 weeks to 1 year, 500ug/kg bd; age 1-4 years, 500ug bd (costing based on 1 tablet per day on the assumption that tablets cannot be carried over to the next day; age 5-12 years, 1-1.5mg bd; age over 13 years, 2mg bd
- b
BNF dose for major depression: by mouth; child 8-17 years, initially 10 mg daily, increased if necessary up to 20 mg daily, dose to be increased after 1-2 weeks of initial dose, daily dose may be administered as a single or divided dose NHS indicative price not reported for Fluoxetine 20mg/5ml sugar free oral solution
- c
Costing based on 1 dispersible tablet or capsule per day on the assumption that tablets cannot be carried over
- d
Low dose costing based on: tablets, 20mg/day; drops, 16mg/day
- e
Max. dose costing based on: tablets, 40mg/day; drops, 32mg/day
- f
BNF dose for major depression: by mouth; child 12-17 years, initially 10 mg once daily, increased if necessary to 20 mg once daily, dose to be increased over 2-4 weeks; maximum 40 mg per day
- g
BNF dose for major depression: by mouth using oral drops; child 12-17 years, Initially 8 mg once daily, increased if necessary to 16 mg once daily, dose to be increased over 2-4 weeks; maximum 32 mg per day
- h
BNF dose for obsessive-compulsive disorder: by mouth; child 6-11 years, initially 25 mg daily for 1 week, then increased to 50 mg daily, then increased in steps of 50 mg at least every 1 week if required; maximum 200 mg per day; child 12-17 years, Initially 50 mg daily, then increased in steps of 50 mg at least every 1 week if required; maximum 200 mg per day
- i
BNF dose for major depression: by mouth; child 12-17 years, initially 50 mg once daily, then increased in steps of 50 mg at least every 1 week if required; maximum 200 mg per day
- j
BNF dose for depressive illness (but not recommended): by mouth, child 6-17 years, initially 10-25 mg 3 times a day, alternatively initially 30-75 mg once daily, dose to be taken at bedtime, increased if necessary to 150-200 mg daily, dose to be increased gradually
- k
Costing based on 1 50mg tablet plus 1 25mg tablet
- l
BNF dose for anxiety (short-term use): by mouth; adult, 5 mg 2-3 times a day, increased if necessary up to 45 mg daily, dose to be increased at intervals of 2-3 days; usual dose 15-30 mg daily in divided doses
G.7.4. Conclusions
The cost of CBT and psychotherapy will ultimately depend on the number of sessions a child or young person with cerebral palsy requires. If those techniques can be successfully replicated at home without the assistance of a health care professional the cost would be substantially less.
According to the BNF, buspirone is an anxiolytic treatment that should be limited to the lowest possible dose for the shortest possible time. It is thought to act at specific serotonin (5HT1A) receptors, although the safety and efficacy in children have yet to be determined. When compared to antidepressants in tablet or capsule form, buspirone tablets are more expensive at around £10 to £13 per month compared to £1 to £5 per month for antidepressants.
Oral solutions of antidepressants are substantially more expensive than capsules or tablets. Therefore, when capsules or tablets can be tolerated they should be offered instead of oral solutions because they are cheaper and there is no evidence to suggest they are any less effective. If an oral solution is required, citalopram would the cheapest at a cost of up to £10 per month.
When the cheapest preparation is chosen, diazepam (2mg tablets), fluoxetine (20mg capsules) and citalopram (20mg or 40mg tablets) are the cheapest antidepressants costing up to £2 per month, whilst sertraline (100mg tablets) and amitriptyline (50mg tablets) cost slightly more. However, in the absence of data on the effectiveness of pharmacological treatments, the cost-effectiveness relative to any of the interventions included in this review cannot be ascertained.
The Committee’s discussion regarding the associated economic benefits and harms are reported in Section 25.6.3 ‘Evidence to recommendations’.
G.8. In children and young people with cerebral palsy, what interventions are cost-effective in optimising saliva control?
G.8.1. Literature review
No economic evaluations of interventions to manage drooling were identified in the literature search conducted for this guideline.
G.8.2. Background
Drooling can significantly impact a person’s health by increasing the risk of infection and risk of choking, and their quality of life; in participation, communication, and eating. There are a number of different drugs available for managing saliva control. A number of them are used for treating other conditions but with saliva control as a side effect. There are a number of clinical approaches ranging from physical therapy and transdermal hyoscine hydrobromide to more invasive interventions such as botulinum toxin type A injections and surgery which have the potential to be high cost.
Unfortunately, there is insufficient evidence to accurately estimate the cost-effectiveness of interventions for drooling, particularly in relation to efficacy. The comparative evidence on interventions to optimise saliva control were generally of poor quality and side-effects profiles did not reflect those observed in UK clinical practice according to the Committee. Moreover, none of the studies included in the clinical review compared physical/postural, oro-motor and oro-sensory therapies, intra-oral appliances, or acupuncture. Where there was more than 1 study reporting the effectiveness of the intervention it was not thought appropriate to synthesise these data due to the various scales used to measure the severity and/or frequency of drooling, and/or the time after intervention when the outcome was measured.
As there is insufficient evidence to suggest better clinical effectiveness with anticholinergic drugs, botulinum toxin type A or surgery, then there is a rationale for recommending transdermal hyoscine hydrobromide over those interventions if they are tolerated by the child or young person with cerebral palsy as they are cheaper, provided transdermal hyoscine hydrobromide themselves are cost-effective relative to “no treatment”. However, the alternatives may not, in fact, be equally effective. If transdermal hyoscine hydrobromide were to prove the more effective option then the economic case would be clear cut, with transdermal hyoscine hydrobromide dominating the alternative interventions (cheaper and more effective). However, if anticholinergic drugs, botulinum toxin type A or surgery were more effective, then the cost-effectiveness would depend on whether the additional benefit was worth the additional cost.
For these reasons, the evaluation took the form of a “what-if” approach to cost-effectiveness analysis to guide recommendations. The Committee members could use such results in conjunction with their clinical judgement to ascertain the likely cost-effectiveness of available interventions. This could then form the basis of a practice or research recommendation.
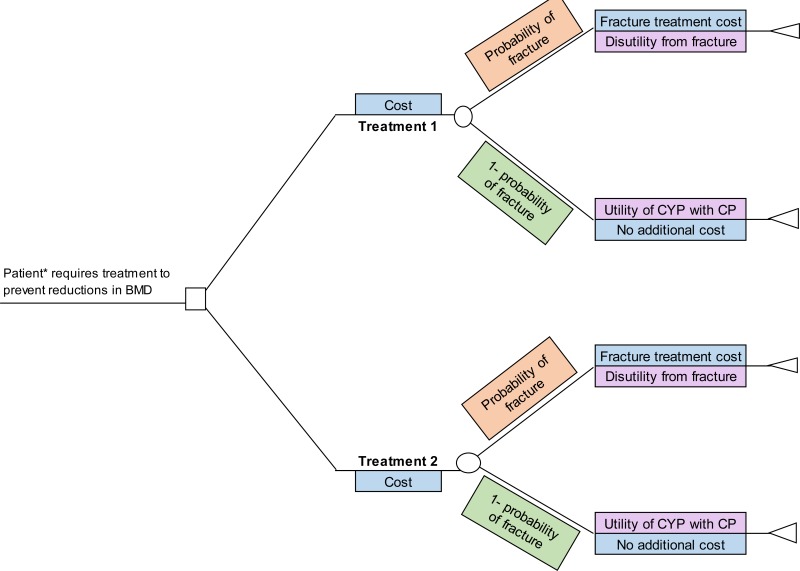
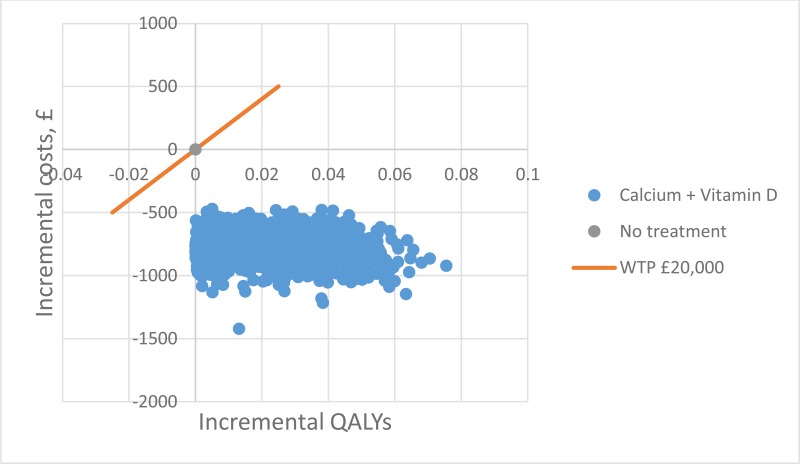
G.8.3. Method
A model was developed in Microsoft Excel® in order to evaluate the cost-effectiveness of interventions in optimising saliva control. The results are presented in term of the QALY gain necessary (based on resource and cost use data alone) and in terms of incremental cost-effectiveness ratios (ICER) where effectiveness is informed by hypothetical health state utilities on a drooling scale (See Section G.8.3.1). For the latter, the results can be presented as either pair-wise comparisons (i.e. 2 interventions) or as a fully incremental analysis where the user can choose the number of intervention to include (i.e. 3 to 5 interventions).
The following interventions available for children and young people who drool were included in the model:
- transdermal hyoscine hydrobromide (Scopoderm patches);
- botulinum toxin type A (Botox®);
- glycopyrronium bromide (glycopyrrolate);
- submandibular duct rerouting surgery.
As the Committee did not consider the routine use of behavioural therapy and benzatropine (anticholinergic drug) to treat drooling, these interventions were not included.
It is important to note that the clinical evidence is highly uncertain, therefore the results from the model should be interpreted with caution. Furthermore, the uncertainty does not relate (primarily) to sampling variation, as for many inputs there is the lack of any evidence base. Therefore, probabilistic sensitivity analysis was not undertaken as meaningful distributions for model inputs could not be estimated. However a series of scenario analyses were undertaken in order to test how sensitive the results were to uncertainty in individual parameters. Parameters varied in the scenario analysis were chosen on the basis of uncertainty in their estimation or the potential impact that they had on the results (Section G.8.3.4 and Section (a))
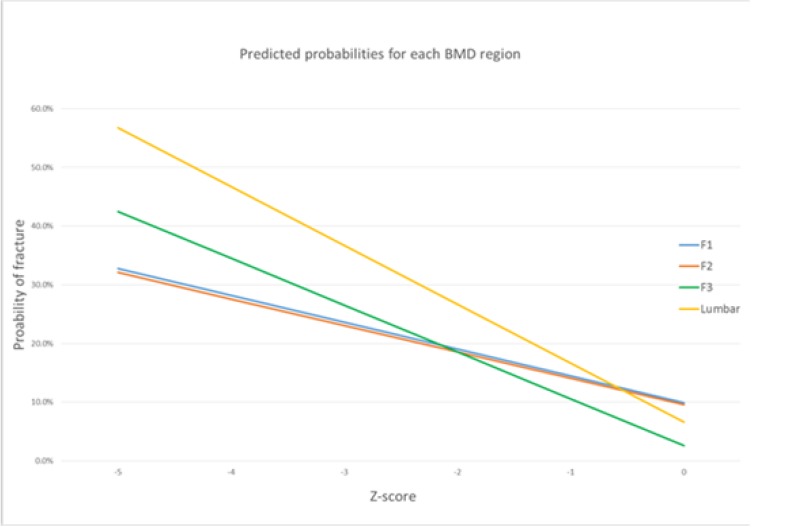
G.8.3.1. Clinical effectiveness
Time horizon
The studies measured clinical effectiveness at different lengths of follow-up, ranging from 2 weeks to 6 months. In the base case a time horizon of 6 months was used to reflect the longest trial duration included in the clinical evidence review. Moreover, the Committee advised that the quantitative and qualitative benefit of botulinum toxin type A is reported between 1 and 6 months with maximum benefit at 4 to 6 weeks post-injection, with some children and young people with cerebral palsy receiving a subsequent injection after 6 months.
Unlike pharmacological interventions, surgery is a one-off procedure. For this reason it is evident that when shorter durations are explored, the benefits and costs of surgery may be underestimated and overestimated, respectively. However in some cases, interventions can resolve drooling problems evading the need for a lifetime intervention. To account for this uncertainty, additional analyses using an 8 week time horizon and lifetime horizon (where costs and benefits were discounted at 3.5% /year) were explored. Due to insufficient evidence to suggest otherwise it is assumed the effects reported in the trials are maintained over the time horizon applied in the model.
Outcome measure
Studies included in the clinical evidence review reported the frequency and/or severity of drooling using one or more of the following measures:
- Thomas-Stonell and Greenberg scale (TSG);
- Teacher Drooling scale (TDS);
- Modified Teacher Drooling scale (mTDS);
- Drooling Impact scale (DIS);
- Drooling quotient;
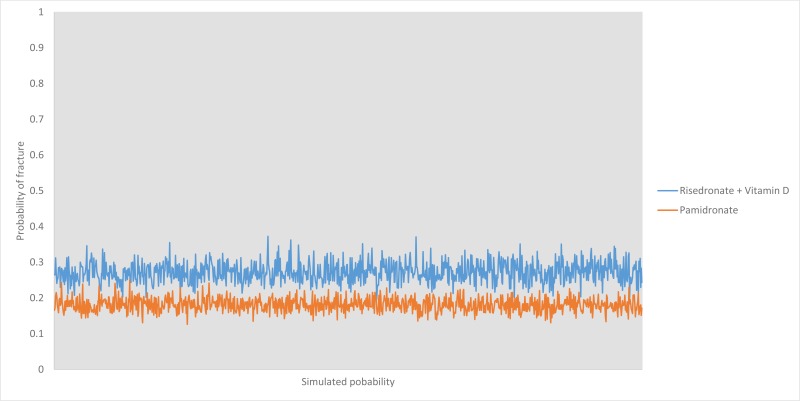
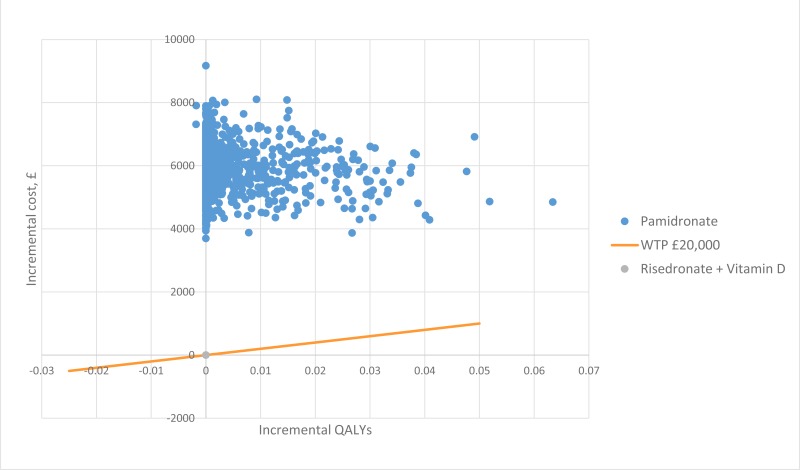
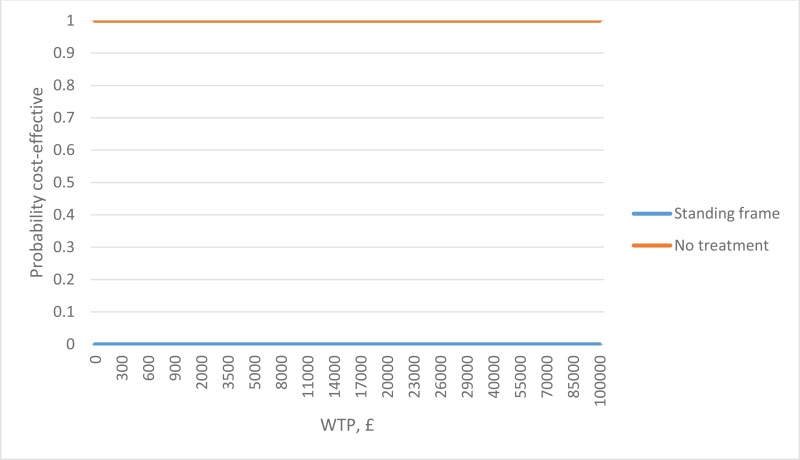
- Drooling Severity and Frequency Scale (DSFS).
It is important to note that the studies included in the clinical evidence review did not consistently define the type of scale or items within the scale they completed, consequently meta-analysis could not be undertaken.
A 9-point TSG scale Table 19 was used to inform the model because this was the most common scale used in the studies. However, the Committee highlighted that the DIS (10 domains with 10 levels) is being used more frequently than the TSG scale in UK clinical practice. They also noted that combining the levels for frequency and severity into a 9-point scale is somewhat misleading as it is unclear which domain the score is driven by. However, they accepted that mapping improvements from the clinical evidence review from the TSG scale on to the DIS scale may lead to even further inaccuracies in clinical effectiveness.
Table 199-point drooling scale
| Score | Description |
|---|---|
| 1 | Dry: never drools; occasionally |
| 2 | Mild: only the lips are wet; occasionally |
| 3 | Mild: only the lips are wet; frequently |
| 4 | Moderate: wet on lips and chin; occasionally |
| 5 | Moderate: wet on lips and chin; frequently |
| 6 | Severe: drools to the extent that clothing becomes damp; occasionally |
| 7 | Severe: drools to the extent that clothing becomes damp; frequently |
| 8 | Profuse: clothing, hands, tray and objects become wet; occasionally |
| 9 | Profuse: clothing, hands, tray and objects become wet; frequently |
In the absence of consistent evidence to inform effectiveness the mean improvement for each intervention was estimated based on assumptions from the literature, and, in sensitivity analysis, according to the views of the Committee.
In the model there are 2 user inputs used to estimate effectiveness:
- drooling score prior to intervention;
- mean improvement in drooling score.
It was assumed children and young people with cerebral palsy seek drooling management for moderate to severe drooling (i.e. a score from 5 to 9) as this reflected the inclusion criteria and baseline scores in the trials (Table 20). In the base case this was set to 7, but this could be varied by the user in the model. The post-intervention score for each intervention was then calculated based on the mean improvement.
The mean improvements used to inform the base-case (or default) ICERs are presented in Table 20. It was assumed that the mean improvement does not depend on the duration of treatment or patient characteristics. The model also assumed effectiveness was independent of time because there was insufficient time-to-event data reported in the studies for this to be a reliable approach to adopt.
Table 20Base-case mean improvement in drooling score
| Intervention | Mean improvement | Rationale |
|---|---|---|
| No treatment | 0 | Drooling severity is assumed to remain constant without management. |
| Transdermal hyoscine hydrobromide | 3 | Parr 2016 included participants with a baseline DSFS score of 7.6, this was reduced for transdermal hyoscine hydrobromide at week 4 by 2.6 and at week 12 by 2.9. |
| Glycopyrrolate | 3 | Zeller 2002 included participants with problem drooling (defined as drooling in the absence of interventions such that clothing became damp approximately 5-7 days a week). The mean reduction in frequency and severity of drooling using the 9-point mTDS scale at 8 weeks was 3.23 higher than placebo (1.89 to 4.57 higher). Mier 2000 included participants with severe sialorrhoea. The mean reduction of frequency and severity of drooling using the 9-point TSG scale at 8 weeks was 4.98 lower than placebo (0 to 0 higher). Parr 2016 included participants with a baseline DSFS score of 7.6, this was reduced for glycopyrrolate at week-4 by 3.0 and at week 12 by 2.9. |
| Botulinium toxin type A | 4 | Reid 2008 included participants with a significant problem with drooling. The mean reduction of frequency and severity of drooling using the drooling impact scale (10-item, 10-point, 100 maximum score) at 4 weeks to be 27.38 higher than no treatment (17.44 to 37.31) Lin 2008 included participants with severe drooling, patients had a baseline score of 6.17 and 6.86 on the TSG scale for the intervention and placebo groups, respectively. The mean reduction of frequency and severity of drooling using the 9-point TSG scale at 4 weeks was 1.54 higher than placebo (0 to 0 higher). Alrefai 2009 included participants with severe drooling scores (≥ 7 on the TSG scale). The mean severity of drooling and mean frequency drooling using the 9-point TSG scale at 4 weeks were both significant (p<0.05) compared to than placebo. Wu 2011 included participants with a chronic drooling problem. The mean reduction of frequency and severity of drooling using the subjective 5-point drooling scale at 4 weeks was not significant (p>0.05) compared to placebo. |
| Surgery (SMDR) | 6 | Based on a prior intervention score of 7, surgery is assumed to fully resolve drooling. Scheffer 2010 reported successful surgery at 32 weeks in 84% of participantsa. |
DSFS, Drooling Severity and Frequency Scale; mTDS, modified Teacher Drooling Scale; SA, sensitivity analysis; SMDR, submandibular duct rerouting; TSG, Thomas-Stonell and Greenberg scale
- a
Successful therapy defined as a 50% reduction in the drooling quotient
G.8.3.2. Measurement and valuation of health effects
The quality adjusted life year (QALY) is NICE’s preferred measure of benefit for economic evaluation. This is because it can be seen as a generic measure of health which allows a comparison across interventions which affect different dimensions of health.
The QALY reflects the 2 principle objectives of health care:
- increase longevity;
- increase quality of life.
Estimating a QALY involves placing a quality of life weight on a particular health state. This quality weight lies between 0 and 1, where 1 denotes full or ‘perfect health’ and 0 denotes death. For this review question hypothetical quality of life weights and health states based on a 9-point drooling scale have been estimated.
In the model there is 1 user input to consider when estimating the quality of life in children and young people who drool: the disutility associated with increasing scores.
A separate systematic search to identify utility values for children and young people with cerebral palsy was not undertaken. Instead, a search was conducted on the CEA Registry using the term “cerebral palsy” in July 2015. This search identified 4 studies with health states relevant to cerebral palsy (Cahill 2011; Obido 2009; Heintz 2008; Carroll 2006). After title and abstract screening only 1 of those studies identified considered people with cerebral palsy, subsequently the full-text of Heintz 2008 was obtained and assessed for inclusion.
Heintz 2008 estimated QALY weights for individuals diagnosed with cerebral palsy based on the utility values reported in the study by Rosenbaum 2007. Consequently the full-text of Rosenbaum 2007 was retrieved and assessed to inform the utility weights in the model.
Rosenbaum 2007 asked carers to complete the Health Utilities Index Mark 3 (HUI3) – a quality of life survey - on behalf of the person with cerebral palsy they cared for. The resulting score was then transformed into a utility value based on an algorithm using Canadian population values. The utility scores estimated for 192 people with cerebral palsy according to their GMFCS level are presented in Table 21.
Table 21Utility values according to GMFCS level
| GMFCS | Number of people with CF | Utility value |
|---|---|---|
| Level I | 60 | 0.84 |
| Level II | 33 | 0.50 |
| Level III | 27 | 0.39 |
| Level IV | 46 | 0.16 |
| Level V | 30 | -0.08 |
CF, cerebral palsy; GMFCS, gross motor function classification system
The methods used to derive utility values within Rosenbaum 2007 are not in line with the NICE reference case which specifies patients to measure their own quality of life using the EQ-5D valued by a representative sample of the UK population. However in the absence of alternative values this study was considered the best available to inform the model. As can be seen from Table 21 a higher GMFCS level is associated with a lower utility value which reflects a lower quality of life. The Committee noted that utility values of 0.16 and -0.08 were very low for children and young people who require physical assistance for mobility. Following this, the Committee believed utility values would be higher if children and young people with cerebral palsy completed the questionnaire themselves.
In the model the GMFCS level and associated utility value represents the highest achievable utility which would represent a drooling score of 1. In the base-case this was set to GMFCS level II associated with a utility of 0.50 which the Committee believed to represent the quality of life of children and young people with cerebral palsy.
Chang 2012 investigated health-related quality of life using the Paediatric Quality of Life Inventory Version in 47 children with cerebral palsy, with and without drooling according to the TSG score. They found the physical health and psychosocial health summary scores of the children that drooled (16.29 ± 15.97 and 42.92 ± 17.57, respectively) were lower than for the children that did not drool (31.97 ± 22.22 and 57.09 ± 12.21, respectively; P < 0.01) concluding the more severe the drooling was (without considering the type of cerebral palsy), the lower the physical and psychosocial quality of life was in the children with cerebral palsy. However the definition of drooling is unclear and this is not disaggregated according to the TSG score. Ideally further research should be conducted using the EuroQol Group’s EQ-5D instrument (a child-friendly version is available) or the Health Utilities Index (which was developed for children) designed to allow subgroup analysis by severity of cerebral palsy in terms of the GMFCS level and drooling score.
It was assumed that the QALY loss from drooling would increase as the drooling score increases. In the model a disutility per unit increase in score was applied additively to the upper utility value. In the base case the disutility was set to an arbitrary value of 0.025, based on 5% of the utility value for GMFCS level II, but the disutility could be adjusted by the user in the model.
Regardless of the disutility value chosen, a linear relationship with the drooling score is maintained, due to insufficient evidence to suggest otherwise. To reiterate, effectiveness is informed by hypothetical health state utilities, but the structure of the model will allow future research to be incorporated.
The base case health state utilities informed by a disutility of 0.025 (per unit increase in score) and GMFCS level II are presented in Table 22. If we compare no drooling to profuse drooling the utility value is almost halved (0.50 vs. 0.30), somewhat reflecting the physical health summary scores reported by Chang 2012 (31.97 vs. 16.29).
Table 22Health state utilities
| Score | Description | Utility value |
|---|---|---|
| 1 | Dry: never drools; occasionally | 0.500 |
| 2 | Mild: only the lips are wet; occasionally | 0.475 |
| 3 | Mild: only the lips are wet; frequently | 0.450 |
| 4 | Moderate: wet on lips and chin; occasionally | 0.425 |
| 5 | Moderate: wet on lips and chin; frequently | 0.400 |
| 6 | Severe: drools to the extent that clothing becomes damp; occasionally | 0.375 |
| 7 | Severe: drools to the extent that clothing becomes damp; frequently | 0.350 |
| 8 | Profuse: clothing, hands, tray and objects become wet; occasionally | 0.325 |
| 9 | Profuse: clothing, hands, tray and objects become wet; frequently | 0.300 |
If the drooling score holds a linear relationship between the score and utility value, the GMFCS level will have no effect on the incremental change in QALYs between interventions because this is not intervention dependent; in other words the QALY gain will change proportionally for each intervention. For example, if we compare glycopyrrolate with a mean improvement of 3 to botulinium toxin type A with a mean improvement of 4 the incremental QALYs over 1 year are 0.025 regardless of the GMFCS level, this is illustrated below for GMFCS levels I and III:
- GMFCS level I:
- 0.075 QALYs gained from glycopyrrolate (post-treatment utility, 0.765 – pre-treatment utility, 0.690)
- 1.00 QALYs gained from botulinium toxin type A (post-treatment utility, 0.790 - pre-treatment utility, 0.690)
- incremental difference of 0.025 (1.00 – 0.075) QALYs.
- GMFCS level III:
- 0.075 QALYs gained from glycopyrrolate (post-treatment utility, 0.315 - pre-treatment utility, 0.240)
- 1.00 QALYs gained from botulinium toxin type A (post-treatment utility, 0.34 - pre-treatment utility, 0.240)
- incremental difference of 0.025 (1.00 – 0.075) QALYs.
Changing the disutility value could have an impact on the recommendations because the larger the disutility value the larger the QALY gain - implying a more cost-effective intervention. This will be a proportionate change i.e. doubling the disutility value will double the hypothetical QALY gain, but changing the disutility value will not impact on the ordering of recommendations - only their cost-effectiveness relative to the NICE threshold.
In the model it is implicitly assumed that all interventions have an identical side effect profile. Were this not the case, differences in morbidity would also have to be incorporated into calculating the differential QALY between these interventions. However, due to insufficient side effects profiles reported within the trials this has to be acknowledged as a limitation of the model.
G.8.3.3. Resource and cost use
In accordance with the NICE Guidelines Manual costing was undertaken from the perspective of the NHS and personal social services (PSS). Drug acquisition cost were taken from the October 2016 NHS Electronic Drug Tariff whilst procedures and attendances were taken from NHS Reference Costs 2014/15, unless otherwise stated.
The acquisition cost of glycopyrrolate depends upon a person’s weight. In addition, the duration of treatment for transdermal hyoscine hydrobromide and glycopyrrolate will vary depending on their response. To cost these treatments accurately there are inputs in the model to vary both the weight (kg) of the child or young person with cerebral palsy and time horizon (weeks). In the base case this is set to 47kg and 26 weeks to reflect the trials included in the clinical evidence review. To explore the impact treatment duration has on cost-effectiveness, sensitivity analyses have been conducted where the duration of treatment is increased to lifetime (40 years) and decreased to 8 weeks.
Transdermal hyoscine hydrobromide (Scopoderm patches)
Table 23 presents the acquisition cost of transdermal hyoscine hydrobromide over the course of 1 day and 1 month of continued use. Based on dosages recommended in the BNF it was assumed children with cerebral palsy aged 3 to 9 years receive 500 micrograms every 72 hours (half a patch) whereas children and young people with cerebral palsy ≥10 years receive 1 mg every 72 hours (1 patch). Despite the difference in dosage, the cost for all people receiving transdermal hyoscine hydrobromide would be equal to 1 patch because patches should not be cut to titrate the dose, instead the time the patch is in contact with the skin is varied..
In clinical practice children and young people with cerebral palsy are not routinely monitored to assess their response to transdermal hyoscine hydrobromide, but they are likely to be seen by their GP surgery once every 6 months (£14 per 15 minute visit, PSSRU 2015). Children and young people with cerebral palsy are assumed to acquire additional prescriptions without a consultation between those visits.
As can be seen from Table 23 transdermal hyoscine hydrobromide provided over a short time-period is relatively inexpensive.
Table 23Acquisition cost of transdermal hyoscine hydrobromide
| Intervention | Basic price, quantity | Unit cost | Cost per day | Cost per week | Cost per month |
|---|---|---|---|---|---|
| Scopoderm 1.5mg patches, 1mg/72 hours | £4.52, 2 patches | £2.26 | £0.75a | £5.25 | £21.00 |
- a
assuming 1 dose lasts 72 hours
Glycopyrrolate
In clinical practice the dose of glycopyrrolate would be adjusted according to response. For a person aged from 1 month to 18 years the BNF recommends 40–100 micrograms/kg (max. 2 mg) 3–4 times daily. Dosage variability was also present in the clinical review:
- Mier 2000 commenced participants <30 kg on 0.6 mg increasing weekly to 1.2 mg, 1.8 mg, and 2.4 mg and children >30 Kg on 1.2 mg, increasing weekly to 1.8 mg, 2.4 mg and 3.0 mg, the dose was given 3 times daily in morning, early afternoon and evening;
- Zeller 2002 commenced participants on 0.02 mg/kg 3 times a day, titrated according over a 4-week period to optimal response, with a maximum dose of 0.1 mg/kg or 3 mg, 3 times a day.
Table 24 presents the drug acquisition cost of glycopyrrolate over the course of 1 dose and a typical weekly and monthly cost of continued use. It is evident from Table 24 that a tablet preparation is substantially more expensive than an oral solution. Given that the NICE guideline manual states that the reference case should reflect the best price available to the NHS, the oral solution (1mg/5ml) is used to inform the model; however, both preparations are included in the model for completeness. It is important to note that other forms such as capsules, oral suspension, oral solution, liquid, cream and ointment are available from special-order manufacturers.
Taking into account the views of the Committee and a paper by Fairhurst and Cockerill 2011 it was assumed children and young people with cerebral palsy who weigh <25kg would receive 1mg twice a day, whereas those who weigh ≥25kg receive 1mg 3 times a day. However, in clinical practice the dose also depends on their response and how bad the drooling was when the intervention was initiated. For this reason a sensitivity analysis was conducted varying the cost of glycopyrrolate by ±50% (Section G.8.3.4 and Section (a)).
Similarly to transdermal hyoscine hydrobromide, children and young people with cerebral palsy are not routinely monitored to assess their response glycopyrrolate; instead families are given a range to work with incurring a routine GP visit every 6 months (£14 per 15 minute visit, PSSRU 2015).
Table 24Acquisition cost of glycopyrrolate according to weight
| Cost according to weight | Basic price, quantity | Unit cost | Cost per day | Cost per week | Cost per month |
|---|---|---|---|---|---|
| Tablets | |||||
| <25Kg, 1mg bd | £214.83, 30 tablets | £7.16 | £14.32 | £100.25 | £401.02 |
| >25Kg, 1mg tds | £214.83, 30 tablets | £7.16 | £21.48 | £150.38 | £601.52 |
| Oral solution (1mg/5ml) | |||||
| <25kg, 1mg bg | £91.00, 150ml | £3.03 | £6.07 | £42.47 | £169.87 |
| >25kg, 1mg tds | £91.00, 150ml | £3.03 | £9.10 | £63.70 | £254.80 |
bd, twice daily; tds, three times daily
Botulinum toxin type A
Table 25 presents the acquisition cost and resource use associated with Botox®. Dysport® is another botulinum toxin type A that can be used to treat drooling, but this was not included as a comparator in the clinical evidence review; moreover, the Committee agreed Botox® is the most common botulinum toxin type A used to treat drooling.
Optimising saliva control is an off-license use of botulinum toxin type A. For this reason, botulinum toxin type A is administered in specialist tertiary centres; often by a specialist consultant guided by ultrasound. The model assumes children and young people with cerebral palsy receive 1 dose of botulinum toxin type A every 6 months.
Table 25Cost of botulinum toxin type A per 6 month administration
| Resource and cost use | Price | Source |
|---|---|---|
| Botox® Injection 50U VL | £77.50 | BNF October 2016 |
| Administration by a neurodisability specialist | £451.50 | NHS Reference Costs 2014/15. Consultant led, Paediatric Neuro-disability 291, Non-Admitted Non Face to Face Attendance, First, WF01B |
| Ultrasound | £92.89 | NHS Reference Costs 2014/15. Ultrasound Scan, Ear, Nose and Throat service 120, MA36Z |
| Total cost | £621.89 | Calculated |
BNF, British National Formulary; VL, vial
The Committee also advised that children and young people with cerebral palsy may be sedated during the procedure. Subsequently the resources for sedation including midazolam (BNF, 10mg/2ml solution for injection, £0.63/ampoule), consumables and an anaesthetist were explored in sensitivity analysis (Section G.8.3.4 and Section (a)). The cost of consumables and an anaesthetist were taken from NICE CG112 (Sedation in under 19s: using sedation for diagnostic and therapeutic procedures) and inflated from 2007 prices to 2015 prices using the hospital & community health services (HCHS) index (293.1 [2015 PPI] / 249.8 [2007 PPI]).
Surgery
The Committee considered a role for surgery (submandicular duct rerouting) in the event of failure of efficacy or intolerance of pharmacological management or botulinum toxin type A injections. It was assumed that this procedure would be performed as an inpatient procedure by an Ear, Nose and Throat service costing £2,286 (NHS Reference Costs 2014/15, CA83C, Elective Inpatient, Major, Mouth or Throat Procedures, 18 years and under).
G.8.3.4. Sensitivity analysis
A series of scenario analyses were undertaken in order to test how sensitive the results were to uncertainty in individual parameters. Parameters varied in the scenario analysis were chosen on the basis of uncertainty in their estimation or the potential impact that they had on the results. The values varied, along with their rationale are shown in Table 26.
Table 26Description of sensitivity analysis
| Scenario analysis, parameter(s) to be changed | Default parameter value | Value tested | Rationale |
|---|---|---|---|
| 1 Clinical effectiveness of botulinium toxin type A | Mean improvement in the drooling score of 4 | Mean improvement increased to 5 | The Committee believed the effectiveness of botulinum toxin type A could be underestimated in the base-case. |
| 2 Total cost of glycopyrrolate | £1,656 /6 months | 50% increase and decrease | The total cost of glycopyrrolate depends upon a person’s weight and their response which cannot be sufficiently captured in the model. |
| 3a Duration of intervention | 6 months | Lifetime (40 years) where costs and benefits are discounted at 3.5% /year | A duration of 6 months reflects the maximum duration of botulinum toxin type A benefit attainable and is the maximum follow-up seen in the trials. In clinical practice the duration is individualised and lifetime in some cases. Although there have been no general studies of life expectancy in people with cerebral palsy, most children affected by cerebral palsy live between 30 and 70 years, depending on the severity of the condition according to the Birth Injury Guide. Given surgery was undertaken in the trial by Scheffer 2010 at a mean age of 14 years, 40 years from surgery was considered reasonable to inform the model. |
| 3b Duration of intervention | 6 months | 8 weeks | A duration of 8 weeks reflects a shorter duration applied in the trials. In clinical practice the duration of treatment is individualised. |
| 4 Clinical effectiveness of transdermal hyoscine hydrobromide | Mean improvement in the drooling score of 3 | Mean improvement decreased to 2 | The Committee believed transdermal hyoscine hydrobromide works well initially (during the first few weeks or months), but becomes less effective than glycopyrrolate in the longer term. |
| 5 Cost of sedation added to botulinum toxin type A administrations | Not included | £134:
| Children and young people with cerebral palsy may undergo a sedation incurring the cost of the drug (midazolam [0.5mg/kg to a max. 15mg] considered to be used more commonly than a general anaesthetic for this indication according to the Committee) consumables and an anaesthetist. |
G.8.4. Model validation
Validation was assessed using 2 primary criteria, internal (verification) and external consistency (validation). Internal validity addresses whether the model has been implemented correctly, and examines the extent to which the mathematical calculations are performed correctly and are consistent with the model’s specifications. Face validation helps ensure a model is constructed and used in accord with best available evidence. This process enhances credibility with experts and increases acceptance of results.
Internal validity was assessed by the primary modeller and a second health economist who also completed the Philips Checklist (Table 32). The following areas of the model were checked:
- plausibility and accuracy of inputs and assumptions;
- programming of formulae and macros;
- efficacy and cost parameters were altered to check whether results changed in the expected direction;
- sensitivity analyses using zero and extreme values were undertaken to check whether results changed as expected;
- input parameters in all arms of the model were set at the same value to check whether outputs (costs and QALYs) in all arms became equal.
This validation stage in model development led to several additional user restrictions in the model. For example when the baseline drooling score is set to 7, the user cannot increase the mean improvement for any intervention beyond 6, if this is attempted a message box with the following message appears “Please reconsider the mean improvement, given the prior intervention score”.
Additionally, members of the Committee validated whether the setting, population, interventions, outcomes, assumptions, and time horizons correspond to those of the decision problem.
G.8.5. Results
The results are presented in terms of the QALY gain necessary based on resource and cost use data alone to determine the additional (incremental) benefit that would be needed for each of the interventions to be considered as the most cost-effective option. The results from the cost-utility analysis informed by hypothetical health state utilities on a 9-point drooling scale are also presented.
If there is strong evidence that an intervention dominates the alternatives (that is, it is both more effective and less expensive), it should normally be recommended. However, if one intervention is more effective but also more expensive than another, then the ICER should be considered. Here the ICER is the difference in the mean costs (incremental costs) divided by the differences in QALYs gained (incremental QALYs gained). It is important to note that these estimates of cost-effectiveness are highly uncertain due to the lack of reliable high-quality clinical evidence, therefore the cost-utility analysis should be interpreted with caution.
When comparing multiple mutually exclusive options, a fully incremental approach should be adopted that compares the interventions sequentially in rank order of cost. In the model the user can determine the number of comparators to include in the analysis. However, only the pair-wise comparisons and a fully incremental analysis including all 5 intervention options are presented here.
G.8.5.1. Base case
QALY gain necessary
Table 27 below presents the total cost of the interventions included in the model over 3 time horizons.
Table 27otal intervention costs
| Intervention | Total cost | |||
|---|---|---|---|---|
| 8 weeks | 6 months | Lifetime (40 years) undiscounted | Lifetime (40 years) discounted at 3.5% /year | |
| No treatment | £0 | £0 | £0 | £0 |
| Transdermal hyoscine hydrobromidea | £56 | £151 | £12,040 | £6,438 |
| Botulinum toxin type A | £622 | £622 | £49,751 | £26,608 |
| Surgery | £2,286 | £2,286 | £2,286 | £2,286 |
| Glycopyrrolatea | £524 | £1,670 | £133,626 | £71,460 |
- a
Including a GP visit every 6 months (£14 per 15 minute visit, PSSRU 2015)
To estimate the QALY gain necessary for an intervention to be considered the first step is to calculate the incremental cost of the interventions being compared. For example if we compare glycopyrrolate to transdermal hyoscine hydrobromide over 6 months:
Incremental cost: £1,670 - £151 = £1,520
The 2014 NICE guidelines manual advises that an intervention will generally be considered cost-effective if the incremental cost effectiveness ratio is £20,000 per QALY or less. In other words, the NHS is willing to pay up to at least £20,000 per QALY gained.
Incremental cost ÷ incremental QALY gain = incremental cost per QALY
£1,520 ÷ incremental QALY gain = £20,000
Or, rearranging:
£1,520÷ £20,000 = incremental QALY gain
Incremental QALY gain = 0.076
This means that as long as a child or young person with cerebral palsy gains at least 0.076 additional QALYs as a result of having the more expensive glycopyrrolate, it would still be considered cost-effective relative to transdermal hyoscine hydrobromide.
Table 28 below presents the incremental QALY gain necessary for the remaining comparisons over the 3 time horizons considered in the model.
Table 28QALY gain necessary for a £20,000 WTP threshold
| Intervention ▼vs. ▶ | No treatment | Transdermal hyoscine hydrobromide | Botulinum toxin type A | Surgery | Glycopyrrolate |
|---|---|---|---|---|---|
| Time horizon 6 months | |||||
| No treatment | - | - | - | - | - |
| Transdermal hyoscine hydrobromide | 0.008 | - | - | - | - |
| Botulinum toxin type A | 0.031 | 0.024 | - | - | - |
| Surgery | 0.114 | 0.107 | 0.083 | - | 0.031b |
| Glycopyrrolate | 0.084 | 0.076a | 0.052 | - | - |
| Time horizon lifetime (40 years) | |||||
| No treatment | - | - | - | - | - |
| Surgery | 0.114 | - | - | - | - |
| Transdermal hyoscine hydrobromide | 0.322 | - | - | 0.208c | - |
| Botulinum toxin type A | 1.330 | 1.008 | - | 1.216c | - |
| Glycopyrrolate | 3.573 | 3.251 | 2.243 | 3.459 | - |
| Time horizon 8 weeks | |||||
| No treatment | - | - | - | - | - |
| Transdermal hyoscine hydrobromide | 0.003 | - | - | - | - |
| Botulinum toxin type A | 0.031 | 0.028 | - | - | 0. 005d |
| Surgery | 0.114 | 0.112 | 0.083 | - | 0.088d |
| Glycopyrrolate | 0.026 | 0.023 | - | - | - |
QALY, quality adjusted life year; WTP, willingness-to-pay
- a
Example described
- b
Glycopyrrolate is cheaper than surgery in this scenario, hence additional QALY gains are required for surgery
- c
Surgery is the cheapest intervention in this scenario, hence additional QALY gains are required for its comparators
- d
Glycopyrrolate is cheaper than botulinum toxin type A and surgery in this scenario, hence additional QALY gains are required for its comparators
The ‘what-if’ threshold analysis presented above suggests what additional benefit each intervention is required to provide in order to be considered cost-effective relative to the comparator. Hence, despite higher intervention costs, an intervention could be considered cost-effective if those QALY gains can be achieved. This is not to say that an intervention is cost-effective, but rather it gives the level of clinical effectiveness relative to the comparator that would be necessary given the current differential in cost and NICE’s willingness to pay threshold of £20,000 per QALY.
It is evident from Table 28 that the time horizon will be a key driver of cost-effectiveness as one intervention that requires the smallest QALY gain under one time horizon can require the greatest QALY gain under another. Smaller QALY gains in Table 28 reflect smaller incremental costs between interventions.
Transdermal hyoscine hydrobromide is the cheapest intervention under an 8 week and 6 month time horizon requiring an additional 0.003 and 0.008 QALYs, compared to “no treatment” to be considered cost-effective at 8 weeks and 6 months, respectively. In other words, transdermal hyoscine hydrobromide requires the smallest QALY relative to the other treatments, compared to “no treatment” to be considered the most cost-effective option.
Glycopyrrolate requires the greatest additional benefit to be considered cost-effective under a lifetime horizon. This is expected because glycopyrrolate is the most expensive intervention in this scenario, hence more additional QALYs are required to justify the large additional cost of glycopyrrolate.
The QALY gains necessary from surgery decrease as the time horizon increases as the one-off cost of surgery is overtaken by the ongoing costs from pharmacological intervention. As a result, surgery is the most expensive intervention, requiring the greatest additional benefit for an 8 week time horizon. Conversely, surgery is the cheapest intervention for a lifetime horizon, requiring the smallest QALY gain.
The comparison of greatest interest for the Committee was between transdermal hyoscine hydrobromide and glycopyrrolate. For glycopyrrolate to be considered cost-effective, an additional 0.023, 0.076 or 3.251 QALYs are required over 8 weeks, 6 months or lifetime, respectively. If clinical evidence or experience justifies that this additional benefit over transdermal hyoscine hydrobromide can be achieved, glycopyrrolate could be considered as a cost-effective alternative to transdermal hyoscine hydrobromide.
Cost-utility analysis
Fully-incremental results
Table 29 below presents the total costs, total QALYs and ICERs for each intervention over a 6 month time horizon.
Table 29ully incremental results (base case, 6 month time horizon)
| Intervention | Total cost | QALYs gained | ICER |
|---|---|---|---|
| No treatment | £0 | 0.00 | - |
| Transdermal hyoscine hydrobromide | £151 | 0.038 | £4,013 |
| Botulinum toxin type A | £622 | 0.050 | £37,711 |
| Glycopyrrolate | £1,670 | 0.038 | Dominateda |
| Surgery | £2,286 | 0.075 | £66,564 |
ICER, incremental cost-effectiveness ratio; QALYs, quality-adjusted life years
- a
Glycopyrrolate is more expensive and less effective than botulinium toxin type A
When a fully incremental analysis is presented the interventions are sequentially ranked in order of cost from the least expensive (“no treatment”) to the most expensive (surgery). Interventions that are followed by more expensive and less effective alternatives are excluded. Here glycopyrrolate is dominated (more expensive and less effective) by botulinium toxin type Aand subsequently excluded. ICERs are then re-calculated for the remaining interventions:
- transdermal hyoscine hydrobromide vs. “no treatment”;
- botulinum toxin type A vs. transdermal hyoscine hydrobromide;
- surgery vs. botulinum toxin type A.
Transdermal hyoscine hydrobromide has an ICER of £4,013 compared with “no treatment”. In general, interventions with an ICER of less than £20,000 per QALY gained are considered to be cost-effective. When interventions with an ICER of less than £20,000 per QALY gained are not recommended explicit reasons should be provided. In this instance, for example, there is insufficient evidence for effectiveness and side effects are not included. In addition “no treatment” may not reflect clinical practice if other interventions not included in this analysis (for example, posture and head positioning) are utilised.
The threshold conventionally used by NICE as an upper limit in cost-effectiveness analysis is £30,000. Botulinum toxin type A has an ICER slightly above this; hence judgements about the acceptability of botulinum toxin type A as an effective use of NHS resources will need strong arguments considering the degree of uncertainty around the ICER. For example, considering if improvements in quality of life have been sufficiently captured and if botulinum toxin type A adds distinct substantial benefits that may not have been adequately captured in the measurement of health gain. However, the Committee has noted that the side-effects profiles identified in the clinical evidence review do not reflect clinical practice, potentially overestimating the QALY gains from botulinum toxin type A.
Surgery has an ICER substantially above NICE’s upper threshold and would not be considered cost-effective under a 6 month time horizon. Moreover, surgery is assumed to fully resolve drooling; hence, the benefits on the 9-point drooling scale are unlikely to be underestimated, however the QALY gain might be since the disutility assigned to increasing scores is subjectively set to 0.025 in the base case (see Section G.8.3.2).
Pair-wise results
Table 30 below present the ICERs estimated from the model for each of the pairwise comparisons. All of the interventions included in the analysis could be considered cost-effective compared to “no treatment”. However, when comparing multiple mutually exclusive options, a fully incremental approach should be adopted that compares the interventions sequentially in rank order of cost. Comparisons with a common baseline should not be used for decision-making. Table 30 is only presented for transparency with the model.
Table 30ase case ICER (Cost per QALY gained) pair-wise (6 month time horizon)
| Intervention ▼vs. ▶ | No treatment | Transdermal hyoscine hydrobromide | Botulinum toxin type A | Surgery | Glycopyrrolate |
|---|---|---|---|---|---|
| No treatment | - | - | - | - | - |
| Transdermal hyoscine hydrobromide | £4,013 | - | - | - | - |
| Botulinum toxin type A | £12,438 | £37,711 | - | - | - |
| Surgery | £30,480 | £56,947 | £66,564 | - | £16,418a |
| Glycopyrrolate | £44,542 | Dominated | Dominated | - | - |
- a
Surgery is more expensive and more effective than glycopyrrolate and would be considered cost-effective with an ICER below NICE’s advisory threshold of £20,000
G.8.5.2. Sensitivity analysis
The fully incremental results from analysis described in Table 26 are presented in Table 31.
Table 31esults from sensitivity analysis (fully incremental)
| Intervention | Total cost | QALYs gained | ICER |
|---|---|---|---|
| 1 Clinical effectiveness of botulinum toxin type A increased (6 month time horizon) | |||
| No treatment | £0 | 0.000 | - |
| Transdermal hyoscine hydrobromide | £151 | 0.038 | £4,013 |
| Botulinum toxin type A | £662 | 0.063 | £18,856 |
| Glycopyrrolate | £1,670 | 0.038 | Dominated |
| Surgery | £2,286 | 0.075 | £133,129 |
| 2a Cost of glycopyrrolate increased by 50% (6 month time horizon) | |||
| No treatment | £0 | 0.000 | - |
| Transdermal hyoscine hydrobromide | £151 | 0.038 | £4,013 |
| Botulinum toxin type A | £622 | 0.050 | £37,711 |
| Surgery | £2,286 | 0.075 | £66,564 |
| Glycopyrrolate | £2,506 | 0.038 | Dominated |
| 2b Cost of glycopyrrolate decreased by 50% (6 month time horizon) | |||
| No treatment | £0 | 0.000 | - |
| Transdermal hyoscine hydrobromide | £151 | 0.038 | £4,013 |
| Botulinum toxin type A | £622 | 0.050 | £37,711 |
| Glycopyrrolate | £835 | 0.038 | Dominated |
| Surgery | £2,286 | 0.075 | £66,564 |
| 3a Duration of intervention set to 8 weeks | |||
| No treatment | £0 | 0.000 | - |
| Transdermal hyoscine hydrobromide | £56 | 0.006 | £9,707 |
| Glycopyrrolate | £524 | 0.006 | Dominated |
| Botulinum toxin type A | £622 | 0.008 | £294,263 |
| Surgery | £2,286 | 0.012 | £432,669 |
| 3b Duration of intervention set to lifetime (40 years)a | |||
| No treatment | £0 | 0.000 | - |
| Surgery | £2,286 | 3.315 | £690 |
| Transdermal hyoscine hydrobromide | £6,438 | 1.658 | Dominated |
| Botulinum toxin type A | £26,608 | 2.210 | Dominated |
| Glycopyrrolate | £71,460 | 1.658 | Dominated |
| 4 Clinical effectiveness of hyoscine decreased | |||
| No treatment | £0 | 0.000 | - |
| Transdermal hyoscine hydrobromide | £151 | 0.025 | £6,020 |
| Botulinum toxin type A | £622 | 0.050 | £18,856 |
| Glycopyrrolate | £1,670 | 0.038 | Dominated |
| Surgery | £2,286 | 0.075 | £66,564 |
| 5. Cost of sedation added to botulinum toxin type A administrations | |||
| No treatment | £0 | 0.000 | - |
| Transdermal hyoscine hydrobromide | £151 | 0.038 | £4,013 |
| Botulinum toxin type A | £755 | 0.050 | £48,394 |
| Glycopyrrolate | £1,670 | 0.038 | Dominated |
| Surgery | £2,286 | 0.075 | £61,223 |
ICER, incremental cost-effectiveness ratio; QALYs, quality-adjusted life years
- a
Costs (except surgery) and benefits discounted at 3.5% /year
The duration of treatment is a key driver of cost-effectiveness. Increasing the duration reduces the cost of surgery relative to the other interventions as this incurs a one-off cost, whereas the other interventions incur an ongoing cost. As a result, surgery dominates transdermal hyoscine hydrobromide, botulinum toxin type A and glycopyrrolate under a lifetime horizon. Conversely, when the time horizon is reduced to 8 weeks, surgery has an ICER substantially above NICE’s threshold and would not be considered cost-effective.
The only scenario where transdermal hyoscine hydrobromide would not considered cost-effective is under a lifetime horizon, all remaining scenarios produce an ICER substantially below NICE’s typical threshold of £20,000 per QALY gained. Therefore transdermal hyoscine hydrobromide should be recommended as a first line intervention.
However, if the Committee believes the clinical effectiveness of botulinum toxin type A is underestimated in the base case, scenario 1 demonstrates that the QALY gains and additional cost from botulinum toxin type A, relative to transdermal hyoscine hydrobromide, would be considered cost-effective with an ICER of £18,856. With regards to implementation, this would lead to a large change in clinical practice as there are currently not enough tertiary centres with the ability to perform botulinum toxin type A injections for this indication. Conversely, if children and young people with cerebral palsy require a general anaesthetic at a cost of £134, botulinum toxin type A would not be considered cost-effective relative to transdermal hyoscine hydrobromide with an ICER above NICE’s advisory upper threshold (£48,394). Combing these 2 scenarios (increasing the effectiveness and cost of botulinum toxin type A) would lead to an ICER of £24,179 which is within NICE’s advisory range for cost-effectiveness (£20,000 to £30,000 per QALY gained).
Glycopyrrolate would not be considered as a cost-effective intervention in any of the scenarios tested. For glycopyrrolate to be considered cost-effective under a threshold of £20,000 per QALY gained, the duration of treatment would need to be less than 10 weeks, given the same QALY gains as botulinum toxin type A. However, given that transdermal hyoscine hydrobromide are believed to be at least equally effective in the short-term, transdermal hyoscine hydrobromide would dominate glycopyrrolate as it is cheaper and at least equally effective.
G.8.6. Discussion
Unfortunately there is insufficient evidence to accurately estimate the cost-effectiveness of interventions for drooling, particularly in relation to side effects. The Committee has stressed the side effects profiles reported in the trials do not reflect clinical practice, especially for transdermal hyoscine hydrobromide and botulinum toxin type A. If those side effects were included in the model the cost-effectiveness of those interventions may be reduced.
The Committee has noted that a patient’s response to treatment is not instantaneous with peaks sometimes occurring weeks after administration. Unfortunately the trials did not report sufficient time-to-event data for this approach to be applied in the model.
There is a high level of uncertainty regarding the impact of drooling on health-related quality of life in children and young people with cerebral palsy. The model assumes the disutility is applied additively to increasing scores. However if drooling had a significantly larger impact on a person’s quality of life at a “profuse” level of severity and a negligible impact at a “mild” level the disutility should instead be applied multiplicatively. In this scenario the QALY gain from the intervention would be larger implying a more cost-effective intervention, assuming the child or young person with cerebral palsy had a profuse starting score. In addition, it is assumed the GMFCS level has no impact on the level of disutility, but this may not hold true in reality.
In reality the duration of treatment, and the dosage of glycopyrrolate and transdermal hyoscine hydrobromide a child or young person with cerebral palsy receives depends on their response. Moreover, doses would be titrated at home and occasionally at routine clinic appointments. As a result, the duration of treatment and dosages of glycopyrrolate and transdermal hyoscine hydrobromide applied in the model are uncertain and large drivers of cost-effectiveness in the model. However these issues have been explored in Section G.8.3.4 and Section (a).
G.8.7. Conclusion
If transdermal hyoscine hydrobromide is more effective than glycopyrrolate in the short term and equally effective in the longer term, then it makes sense to recommend transdermal hyoscine hydrobromide as a first line intervention. This is a considerably cheaper option and thereby frees up resources for alternative NHS use and patient benefit. However, if the gains in effectiveness from transdermal hyoscine hydrobromide are reduced from treatment related adverse effects, then recommendations in favour of glycopyrrolate as a first line intervention could be considered if long-term drug treatment is not anticipated
The cost of glycopyrrolate begins to overtake the cost of botulinum toxin type A after approximately 10 weeks of continuous administration; consequently, botulinum toxin type A dominates glycopyrrolate after 10 weeks as it is less expensive and more effective. However, if the gains in effectiveness from botulinum toxin type A are reduced from treatment related adverse effects, then botulinum toxin type A may not be considered cost-effective relative to glycopyrrolate.
In addition, a recommendation in favour of botulinum toxin type A as a second line treatment would require a large injection of resources to implement as only a minority of centres have the ability to administer botulinum toxin type A for this indication. Increasing the supply of specialists would incur an upfront training cost; however, if the benefits obtained from botulinum toxin type A are above the other drug treatments under consideration that would mean that botulinum toxin type A is cost-effective or even cost saving over the medium to long term and so would be recommended for funding.
Increasing the duration of treatment reduces the cost of surgery relative to the other interventions as surgery incurs a one-off cost, whereas pharmacological interventions incur ongoing costs. Therefore, if pharmacological interventions cannot resolve drooling problems and evade the need for lifetime treatment, surgery would be considered cost-effective as it dominates the alternatives. However, surgery is often contraindicated for many children and young people with cerebral palsy and may need repeating if it is performed too young.
The Committee’s discussion regarding the associated economic benefits and harms are reported in Section 17.6.3 ‘Evidence to recommendations’.
Table 32Philips checklist, drooling
| Dimension of quality | Comments |
|---|---|
| Structure | |
| S1: Statement of decision problem/objective | Clearly stated. |
| S2: Statement of scope/perspective | Clearly stated perspective (UK NHS). |
| S3: Rationale for structure | Model structure makes sense given the health condition. Although model type is not explicitly stated. |
| S4: Structural assumptions | All assumptions are transparent. All assumptions were justified except for:
|
| S5: Strategies/ comparators | Options under evaluation are clearly defined. All feasible and practical options are evaluated and justification is provided as to the exclusion of certain potential interventions (behavioural therapy and benzatropine for example Section G.8.3 |
| S6: Model type | Appropriate; cost-utility analysis. |
| S7: Time horizon | Time horizon of 6 months is justified and the difference in the relative costs of interventions that might arise from a lifetime time horizon (or a time horizon less than 6 months) is acknowledged and included in the further analysis. |
| S8: Disease states/pathways | Appropriate and justified |
| S9: Cycle length | Model assumes that treatment effectiveness is independent of time. This seems to be the reason why cycle length is not discussed. |
| Data | |
| D1: Data identification | Data derived wholly from clinical evidence and committee expertise because, as stated, no economic evaluation relevant to condition were identified in literature search. It is clear that data identified is appropriate and justification/explanation is provided when relevant data on important parameters is not included (for example, the lack of data on side effects, which would affect utilities, is explained. Quality of the data is discussed. For example, as it relates to:
|
| D2: Pre-model data analysis | Pre-model data analysis in conducted and methods are transparent. (For example, as it relates to the drooling scale used. |
| D2a: Baseline data | All uncertainty associated with baseline data is tackled in scenario analysis discussed in Table 26. |
| D2b: Treatment effects | It is stated in guideline that it was not thought appropriate to synthesise data on treatment effects. Justification is provided. Assumptions regarding continuing effect of treatment once it has been ceased (or in the case that it is continuous) are provided with justifications. |
| D2c: Costs | Costs are justified and sources are described. Discounting is irrelevant in the base case, |
| D2d: Quality of life weights (utilities) | Sources of utility weights are provided but application/method of incorporation isn’t justified (as previously mentioned). |
| D3: Data incorporation | Data incorporated into the model is justified and source based where possible. Issues with data incorporation are the same issues discussed in section S4 of this checklist. |
| Assessment of uncertainty | |
| D4a: Methodological | Scenario analysis is conducted (as previously discussed). |
| D4b: Structural | Further sensitivity analysis (changing the time horizon to 8 weeks or ‘lifetime’) has been previously discussed. |
| D4c: Heterogeneity | There is no discussion of an assessment of this form of uncertainty. |
| D4d: Parameter | The lack of inclusion of a probabilistic sensitivity analysis is discussed. |
| Consistency | |
| C1: Internal consistency | Internal consistency checks have been conducted in this model as discussed in the model validation section. |
| C2: External consistency | Not assessed. |
CP, cerebral palsy; GMFCS, Gross Motor Function Classification System
G.9. Prevention of reduced bone mineral density
G.9.1. Literature review
No economic evaluations of interventions to prevent reduced bone mineral density (BMD) and low-impact fractures were identified in the literature search conducted for this guideline.
G.9.2. Background
Low BMD has a significant impact on quality of life as it effects posture, ability to walk, and therefore ability to participate. There are a number of clinical approaches ranging from physical therapy to pharmacological treatments which have the potential to be high cost.
Recommendation on treatments to limit reductions in BMD and reduce the low impact fractures arising from low BMD will affect the majority of children and young people with cerebral palsy. Therefore, there is potential for this area of management to have significant resource implications and benefits. For these reasons, a decision prior to the clinical search was made to prioritise this review question for economic modelling.
When presented with the clinical evidence review, the Committee discussed 2 separate populations: children and young people with cerebral palsy at increased risk of reduced BMD, and those with proven osteoporosis.
The Committee noted that osteoporosis is far more prevalent in the more complex population who would be unable to participate in active (weight-bearing) exercise. Moreover, not many osteoporotic people with cerebral palsy would be able to use vibration plates given their postural distortions, physical and cognitive impairments.
The Committee also acknowledged that there was significant evidence to suggest standing frames improve BMD; although they believed standing frames were not frequently used for this purpose.
From this discussion it was evident there were 3 distinct populations the interventions listed in the protocol would apply to:
- Children and young people with cerebral palsy at increased risk of reduced BMD who receive supplementation, or undertake active exercise, or weight-bearing activities;
- Children and young people with cerebral palsy with proven osteoporosis requiring pharmacological treatment (no treatment would not be considered as an option in clinical practice);
- Children and young people with cerebral palsy who use standing frames as part of their postural management programme.
G.9.3. Methods: clinical effectiveness
G.9.3.1. Intermediate to final outcomes
In line with NICE’s preferred method for economic evaluation, a de novo cost-utility model was constructed to determine the most cost-effective interventions for those 3 populations outlined in Section G.9.2.
One outcome to be considered as a possible alternative to quality-adjusted life years (QALYs) was the number of low impact fractures prevented. However, none of the included studies reported on this outcome, and neither did the studies report adverse effects (bone fragility and/or gastric/oesophageal irritation/ulceration). Instead, studies reported on the changes in BMD measured with dual energy X-ray absorptiometry (DEXA) scans at various sites.
BMD is an intermediate outcome that does not incorporate quality or quantity of life. When conducting cost-utility analysis, final endpoints that are related to health related quality of life and hence to utilities and QALYs are required. A link was established between BMD and risk of fracture because the Committee agreed the clinical evidence review on risk factors demonstrated a strong relationship.
A decision tree model was developed in Microsoft Excel® (2013) (Figure 2) from the perspective of the NHS, using 2014/15 costs. For the first 2 populations, the time horizon for the model was a year as this reflected the longest trial follow-up in the clinical evidence review. In addition, those interventions are not generally prescribed on a longer basis due to changes in child or young person’s physique and nutrition, or potential pharmacological toxicities (bisphosphonates). As a result, no discount rate was applied. However, for children and young people with cerebral palsy who use standing frames as part of their postural management programme, the time horizon was increased to 5 years to reflect the lifespan of a standing frame.
Figure 2Decision tree model
* Patient from 1 of 3 defined populations; CYP with CP, children and young people with cerebral palsy
A common algorithm used to evaluate a person’s risk of fracture is the World Health Organisation (WHO) Fracture Risk Assessment (FRAX) tool developed by the University of Sheffield. However, this tool uses BMD measures from the femur neck and is only applicable to people aged 40 years or over. For these reasons the FRAX tool was not considered appropriate for children and young people with cerebral palsy.
To estimate the risk of fracture from BMD, the model utilised an approach used in a study identified in the clinical evidence review (Henderson 2010) who tested the hypotheses that DEXA measures of BMD correlate with bone fractures in children and adolescents with cerebral palsy or muscular dystrophy. This was undertaken by calculating BMD Z-scores for the distal femur and lumbar spine.
Z-scores can be used to compare a measurement to a reference value. The Z-score is the number of standard deviations away from the average value of the reference group using the following formula:
A total of 507 children with cerebral palsy and 112 with muscular dystrophy aged 6 to 18 years from 8 centres in the US, of sufficient severity to significantly impair ambulation, were included in the study by Henderson 2010. Considering that Gross Motor Function Classification System (GMFCS) levels IV and V were identified as risk factors for low BMD in the clinical evidence review, the prevalence of fracture taken from Henderson 2010 would be overestimated if applied to ambulant children i.e. GMFCS levels I to III.
This has to be acknowledged as a limitation for the population with children and young people at increased risk of reduced BMD who will be ambulatory. However, this is unlikely to change the incremental difference between the treatments as the risk would change proportionately for both treatments when they are administered to homogeneous populations.
Henderson 2010 do not specify the type of bone fracture participants experienced. However, they stated that the most common site in healthy children is the forearm, with over 80% of the fractures occurring in the upper limb and fewer than 2% in the femur. They also added that in contrast, over 70% of fractures occur in the lower limb of non-ambulatory children with disabilities such as cerebral palsy or muscular dystrophy, and up to one-half of all fractures are in the femur. The quality of life and implications according to the site of fracture are discussed further in Sections G.9.4 and G.9.5.1.
Table 33 below presents the prevalence of fracture against the anatomical site according to 5 equally sized Z-score groups. It is evident that the probabilities in Table 33 do not follow a linear relationship, however the Committee agreed a linear assumption would be reasonable to inform the model. The prevalence reported was a point estimate. In addition, a participant’s history of prior fracture was obtained at the time of the DEXA scan, but this was categorised into a simple yes, or no, providing no information on the timing or number of fractures participants experienced. Consequently, this has to be acknowledged as a limitation of converting BMD into a probability of fracture for the time horizon in the model. For simplicity, it is also assumed patients can only experience 1 fracture in the model.
Table 33Prevalence of fracture vs. BMD z-score reproduced from Henderson 2010
| Distal femur region 1 (F1) | Distal femur region 2 (F2) | Distal femur region 3 (F3) | Lumbar spine | ||||
|---|---|---|---|---|---|---|---|
| Z-score | % | Z-score | % | Z-score | % | Z-score | % |
| >-1.8 | 13% | >-1.7 | 14% | >-1.4 | 11% | >-1.0 | 17% |
| -1.8 to -3.2 | 23% | -1.7 to -3.0 | 21% | -1.4 to -2.5 | 24% | -1.0 to -1.9 | 26% |
| -3.2 to -4.3 | 33% | -3.0 to -4.5 | 32% | -2.5 to -3.5 | 22% | -1.9 to -2.6 | 20% |
| -4.3 to -5.8 | 37% | -4.5 to -6.5 | 31% | -3.5 to -4.8 | 37% | -2.6 to -3.5 | 39% |
| <-5.8 | 30% | <-6.5 | 39% | <-4.8 | 41% | <-3.5 | 44% |
The ranges in Table 33 were considered to be too restrictive to demonstrate differences between the interventions within the trials and across the trials included in the clinical evidence review. This was because the majority of interventions were found to lie within the same Z-score percentile; hence the interventions would be associated with the same risk of fracture. For this reason the mid-point of each 20th percentile group was taken to inform a linear trend using Microsoft Excel® (2013). This linear trend estimates the risk of fracture for each intervention, subsequently demonstrating differences in their effectiveness that were unobservable from the Z-score ranges in Table 33. The estimated linear trends used to inform the model are illustrated in Figure 3.
Figure 3 illustrates the expected negative relationship between the Z-score and the probability of fracture i.e. as the Z-score gets bigger (more negative) the probability of fracture increases. Using this relationship in the model will enable the probability of fracture to be estimated separately for each intervention, given the Z-score is available for the femur or lumbar spine.
G.9.3.2. BMD sites included in the model
As noted in Section G.9.3.1 Henderson 2010 took DEXA measures from the femur or lumbar spine, whereas the clinical evidence report also reported measures from the femur neck.
To decide what assumptions can be made to allow data to be included given heterogeneity between different BMD sites, the Committee was consulted. This led to 2 assumptions that would incorporate the largest evidence base:
- Distal femur region 1 (F1) used as a proxy for the femur neckThe Committee noted that in UK clinical practice the most common sites used to measure BMD are the femur neck and lumbar spine. However, not all of the studies included in the clinical review reported BMD at those sites. Consequently an assumption was made that the distal femur region 1 (F1) could be used as a proxy for the femur neck as they were considered to be the closest sites in terms of properties and proximity.
- When 3 regions of the distal femur are reported, F1 will be used to inform the modelWhen studies reported regions of the distal femur, all 3 regions (F1, F2 and F3) were reported, as a result F1 would be the region included in the model as this would facilitate the largest number of comparisons (given the previous assumption).
The correlations reported by Henderson 2002b between BMD sites (Table 34) supported these assumptions. They found that the proximal femur (the closest measurement to the femur neck) was highly correlated with each of the 3 regions of the femur, whereas the lumbar spine was less well correlated with the 3 regions of the femur.
The clinical evidence review also found that within the same study, one site would show a significant difference whereas another may not. For these reasons, both the lumbar spine and F1 are included in the model to capture this uncertainty.
Conflicting results in the clinical evidence review included:
- a clinically beneficial effect of increased time spent on the standing frame compared to no increase in the regular standing duration for vertebral BMD, but no clinically significant difference for proximal tibial BMD;
- a significant difference between the 2 groups for areal BMD of the femur, but no significant difference between home-based cycling program and usual physical activity for areal BMD of the lumbar spine,;
- a clinically beneficial effect of pamidronate disodium compared to placebo for BMD in distal femur region 1, 2 and in the lumbar spine, but no clinically significant difference for BMD in distal femur region 3.
Table 34BMD site correlations reproduced from Henderson 2002b
| Anatomic region | Distal femur region 1 (F1) | Distal femur region 2 (F2) | Distal femur region 3 (F3) | Proximal femur | Lumbar spine |
|---|---|---|---|---|---|
| Distal femur region 1 (F1) | 1.00 | - | - | - | - |
| Distal femur region 2 (F2) | 0.94 | 1.00 | - | - | - |
| Distal femur region 3 (F3) | 0.89 | 0.99 | 1.00 | - | - |
| Proximal femur | 0.89 | 0.92 | 0.91 | 1.00 | - |
| Lumbar spine | 0.83 | 0.88 | 0.89 | 0.87 | 1.00 |
G.9.3.3. Baseline adjustments
Inclusion criteria applied by the studies included in the clinical evidence review varied, as a result this led to heterogeneous populations. For this reason, a single baseline pre-treatment BMD was applied to the population at increased risk of reduced BMD and population with proven osteoporosis as study heterogeneity meant that the baseline BMD in the individual studies differed markedly. Inclusion criteria and pre-treatment BMD reported by the studies included in the model are presented in Table 35 for the 3 populations included in the model.
Table 35ummary of study participants, pre-treatment
| Population | Intervention / study | Study inclusion criteria | Pre-treatment BMD | |
|---|---|---|---|---|
| F1 | Lumbar | |||
| At increased risk of reduced BMD | Active exercise (cycling) / Chen 2013 | GMFCS levels I-II | 0.72 | 0.58 |
| Weight-bearing exercise/ Chad 1999 | Spastic CP: 2 independent ambulatory, 6 non-ambulators, 5 ambulators with assistance, 5 independent ambulators with aid | 0.36 | NR | |
| Vitamin D Iwasaki 2008 | CP with secondary osteoporosis | 0.32 | NR | |
| Vitamin D plus calcium/ Jekovec 2000 | Spastic quadriplegia, bedridden and dependent on assisted feeding | NR | 0.38 | |
| Vibration therapy / Ruck 2010 | GMFCS levels II, III, or IV | 0.60 | 0.49 | |
| Proven osteoporosis | Pamidronate/Henderson 2002 | Non-ambulatory with quadriplegic CP | 0.35a | 0.32a |
| Vitamin D plus calcium / Jekovec 2000 | Spastic quadriplegia, bedridden and dependent on assisted feeding | NR | 0.38 | |
| Risedronate plus vitamin D/ Iwasaki 2008 | CP with secondary osteoporosis | 0.45 | NR | |
| Vitamin D / Iwasaki 2008 | CP with secondary osteoporosis | 0.32 | NR | |
| Postural management | Standing frame/ Caulton 2004 | Non-ambulant children with CP | NR | 0.38 |
| “No treatment”/Caulton 2004 | NA | NA | ||
BMD, bone mineral density; CP, cerebral palsy; GMFCS, gross motor function classification system; NA, not applicable; NR, not reported
- a
Calculated from Z-scores reported in the study
To obtain homogeneous populations, the active exercise (cycling) study by Chen 2013 was chosen to inform the baseline BMD for the population at increased risk of reduced BMD, and the study by Henderson 2002 that evaluated pamidronate disodium was chosen for the proven osteoporosis population. Both of these studies included measures for F1 and lumbar spine to ensure the pre-treatment BMD from both sites was adjusted. These studies also included participants that reflected the intended population: ambulatory participants and non-ambulatory participants, respectively.
It is important to note that Henderson 2002 only reported Z-scores, but pre-treatment BMD can be calculated using the following rearrangement of the Z-score:
Henderson 2002 also based the expected BMD for the distal femur on Henderson 2002b which is consistent with the reference data utilised in the model (Section G.9.3.4).
Table 36 below shows the baseline pre-treatment BMD applied to each population.
Table 36djusted pre-treatment BMD
| Population | Baseline study | Pre-treatment BMD, adjusted | |
|---|---|---|---|
| F1 | Lumbar | ||
| At increased risk of reduced BMD | Active exercise (cycling) Chen 2013 | 0.72 | 0.58 |
| Proven osteoporosis | Pamidronate disodium Henderson 2002 | 0.35 | 0.32 |
| Postural management | Standing frame Caulton 2004 | NA | 0.38a |
BMD, bone mineral density; NA, not applicable
- a
Not adjusted, unadjusted pre-treatment BMD 0.38 (lumbar spine)
Further assumptions were required to include the standing frame and vitamin D studies in the model. These studies only reported p values, but it was possible to estimate BMD from the statements that were made within the studies. Because of the estimation techniques used to include these studies, the results inferred must be interpreted with caution.
Caulton 2004 was the only study included in the postural management population, and they reported a 6% mean increase in the vertebral BMD in participants who used standing frames for increased durations. The baseline BMD (0.38) was taken from Jekovec 2000 (calcium and vitamin D), who included participants who had spastic quadriplegia and were bedridden to reflect the non-ambulatory population included in the standing frame study. This was then inflated by 6% based on Caulton 2004 to estimate the post-treatment BMD (0.40).
It is important to note that the comparison analysed in the model was between a standing frame and “no treatment” as this was the comparison of interest to the Committee. For this reason, the additional benefit from an increased standing duration compared to a normal standing duration was assumed to equal the additional benefit of standing frames compared to “no treatment”.
For risedronate plus vitamin D compared with vitamin D, Iwasaki 2008 only reported p values. However, this study was included in the model as a graph presented with a regression line enabled an estimation of pre-treatment BMD (x) and post-treatment BMD (y). The pre-treatment value (x) was arbitrarily chosen from the graph, but the regression line reported by the study means the change in BMD is the same regardless of the baseline value.
Assuming a pre-treatment BMD of 0.32 (x) for vitamin D results in a post-treatment BMD (y) of 0.33 based on the regression line reported by Iwasaki 2008:
Assuming a pre-treatment BMD of 0.45 (x) for risedronate plus vitamin D results in a post-treatment BMD (y) of 0.48:
The regression line was not used to estimate the post-treatment BMD in the base case as this is informed from the relative improvement on the adjusted baseline pre-treatment BMD (Table 66). However, a sensitivity analysis estimated the post-treatment BMD using the regression line.
Iwasaki 2008 undertook a randomised trial, but the 2 arms were not comparable at baseline. For this reason, Iwasaki 2008 compared the 2 arms separately i.e. pre-treatment versus post-treatment.
G.9.3.4. Source of expected BMD to calculate Z-scores
The expected BMD and standard deviation (SD) values to calculate Z-score are only required for the chosen baseline study in each of the 3 populations, not every study included in the model. This is because the expected values reflect a homogenous population defined by the baseline study.
Because a common baseline BMD has been applied to each population, cost-effectiveness is determined from the post-treatment BMD rather than the change in BMD. Moreover, the structure of the decision tree would not enable the change in BMD to be used as an outcome measure.
To calculate the Z-score for each intervention, the participant’s pre-treatment BMD was taken from the mean BMD reported in the baseline study (Chen 2013, cycling/at increased risk of reduced BMD; Henderson 2002, pamidronate disodium /proven osteoporosis; Jekovec 2000 [estimated from Caulton 2004], standing frame) pre-treatment and post-treatment. The DEXA site measured, age and gender of study participants was also recorded to ensure the expected BMD reflected the participants in the trials.
The expected BMD was taken from the National Health and Nutrition Examination Survey (NHANES) 2005-2008. This survey aimed to provide reference values for lumbar spine BMD DEXA measures in a US population in participants aged 8 years and over, disaggregated further by age and nationality.
Henderson 2002b estimated equations to predict distal demur BMD DEXA measures for males and females. This was estimated from 231 Non–African Americans with a mean age of 10.5 years (range 3 years to 18 years 6 months). The equations to calculate the expected BMD and SD for the distal femur region 1 are presented in Table 37. As noted in Section G.9.3.1 this study was used to calculate Z-scores for a correlation study (Henderson 2010) and to calculate Z-scores in a study that included pamidronate disodium as an intervention (Henderson 2002).
Table 37Equations used to predict distal femur BMD according to age, gender and anatomic region reproduced from Henderson 2002b
| Distal femur region | Predicted BMD | SD |
|---|---|---|
| F1 male | 0.64605 + (-0.0054* age) + (0.00219*age2) + (0.000002* age3) | 0.0421* √age |
| F1 female | 0.51291 + (0.02987* age) + (-0.00081*age2) + (0.00008* age3) | 0.0336* √age |
BMD, bone mineral density; SD, standard deviation
In the model the expected BMD and SD was calculated separately for males and females, then weighted according to the proportion of males in the study. Table 38 presents the resulting estimations for expected BMD and SD for the 3 populations.
Table 38Population reference data used to estimate Z-scores
| Population (baseline intervention) | Age | % male | BMD site | Source of reference data | Expected BMD, weighted by gender | Expected SD, weighted by gender |
|---|---|---|---|---|---|---|
| At increased risk of reduced BMD (cycling) | Mean 8.65 years | 69% | Lumbar spine | NHANES non-hispanic white 8 to 11 years | 0.64 | 0.10 |
| F1 | Henderson 2002b | 0.76 | 0.12 | |||
| Proven osteoporosis (pamidronate disodium) | Range 6 to 16 years | 50% | Lumbar spine | NHANES non-hispanic white 8 to 11 years | 0.63 | 0.09 |
| F1 | Henderson 2002b | 0.85 | 0.13 | |||
| Postural management | Mean 7.3 years | 54% | Lumbar spine | NHANES non-hispanic white 8 to 11 years | 0.63 | 0.10 |
BMD, bone mineral density; NHANES, National Health and Nutrition Examination Survey; SD, standard deviation
The difference between the adjusted pre-treatment BMD (common baseline) and unadjusted pre-treatment BMD (study reported) was calculated to find an inflator to apply to the post-treatment BMD. This is described in more detail in Table 64.
Table 39 below presents the adjusted post-treatment BMD scores and resulting Z-scores for each intervention. As stated previously, adjustments to the population at increased risk of reduced BMD were made using active exercise (cycling), and for proven osteoporosis, using pamidronate disodium.
Table 39Z-scores used in the model for each intervention
| Population | Intervention | Post-treatment BMD, adjusted | Z-score | ||
|---|---|---|---|---|---|
| F1 | Lumbar | F1 | Lumbar | ||
| At increased risk of reduced BMD | Active exercise (cycling) | NA | NA | -0.21 | -0.57 |
| Weight-bearing exercise | 0.76 | NA | -0.03 | NA | |
| Vitamin D | 0.74 | NA | -0.18 | NA | |
| Vitamin D plus calcium | NA | 0.73 | NA | 0.99 | |
| Vibration therapy | 0.77 | 0.59 | -0.05 | -0.42 | |
| “No treatment”a | NA | NA | -0.29 | -0.54 | |
| Proven osteoporosis | Pamidronate disodium | NA | NA | -1.80b | -2.20b |
| Vitamin D plus calcium | NA | 0.40 | NA | -2.49 | |
| Risedronate plus vitamin D | 0.38 | NA | -3.79 | NA | |
| Vitamin D | 0.36 | NA | -3.91 | NA | |
| Postural management | Standing frame | NA | NA | NA | -2.39 |
| “No treatment” | NA | NA | NA | -2.62c | |
BMD, bone mineral density; NA, not applicable
- a
Taken from the cycling trial no treatment arm
- b
Reported by Henderson 2002
- c
No treatment taken as standing frame pre-treatment
As expected, the population at increased risk of reduced BMD has the highest Z-scores (less negative) which suggests they are closer to the general population that those with proven osteoporosis or those who require a standing frame.
G.9.3.5. Probability of fracture
Table 40 below presents the probability of fracture calculated for each intervention based on the linear relationship estimated from the study by Henderson 2010 (Section G.9.3.1).
Table 40Probability of fracture for each intervention included in the model
| Population | Intervention | Z-score | Probability of fracture | ||
|---|---|---|---|---|---|
| F1 | Lumbar | F1 | Lumbar | ||
| At increased risk of reduced BMD | Active exercise (cycling) | -0.21 | -0.57 | 10.9% | 12.4% |
| Weight-bearing exercise | -0.03 | NA | 10.1% | NA | |
| Vitamin D | -0.18 | NA | 10.8% | NA | |
| Vitamin D plus calcium | NA | 0.99 | NA | 0%a | |
| Vibration therapy | -0.05 | -0.42 | 10.1% | 10.8% | |
| “No treatment” | -0.29 | -0.54 | 11.3% | 12.1% | |
| Proven osteoporosis | Pamidronate disodium | -1.80 | -2.20 | 18.2% | 28.7% |
| Vitamin D plus calcium | NA | -2.49 | NA | 31.7% | |
| Risedronate plus vitamin D | -3.79 | NA | 27.2% | NA | |
| Vitamin D | -3.91 | NA | 27.8% | NA | |
| Postural management | Standing frame | NA | -2.39 | NA | 30.6% |
| “No treatment” | NA | -2.62 | NA | 32.9% | |
BMD, bone mineral density; NA, not applicable
- a
Calculated as -3.3% and adjusted to 0%
A baseline pre-treatment BMD is applied to all studies in a population; hence, the probability of fracture pre-treatment is equal across the interventions in that population. Consequently, the change in the probability of fracture (pre- vs. post-treatment) is inferred from the probability of fracture post-treatment.
For illustrative purposes the change in the risk of fracture (post-treatment vs. pre-treatment) is presented in Table 41. It is evident that the change in the risk of fracture is small except for vitamin D plus calcium and pamidronate disodium which reflects the findings from the clinical evidence review.
In the base case, the probability of fracture over a 5-year time horizon utilises the probabilities reported in Table 43 as it is unclear from Henderson 2010 the point in time prevalence was measured.
Table 41Change in the risk of fracture
| Population | Intervention | Probability of fracture, pre-treatment | Probability of fracture, post-treatment | Change | |||
|---|---|---|---|---|---|---|---|
| F1 | Lumbar | F1 | Lumbar | F1 | Lumbar | ||
| At increased risk of reduced BMD | Active exercise (cycling) | 11.7% | 12.4% | 10.9% | 12.4% | -0.8% | 0% |
| Weight-bearing exercise | 10.1% | NA | -1.6% | NA | |||
| Vitamin D | 10.8% | NA | -0.9% | NA | |||
| Vitamin D plus calcium | NA | 0%a | NA | -12.4% | |||
| Vibration therapy | 10.1% | 10.8% | -1.6% | -1.6% | |||
| “No treatment” | 11.3% | 12.1% | -0.4% | -0.3% | |||
| Proven osteoporosis | Pamidronate disodium | 28.2% | 40.7% | 18.2% | 28.7% | -10.0% | -12.0% |
| Vitamin D plus calcium | NA | 31.7% | NA | -9.0% | |||
| Risedronate plus vitamin D | 27.2% | NA | -1% | NA | |||
| Vitamin D | 27.8% | NA | -0.4% | NA | |||
| Postural management | Standing frame | NA | NA | NA | 30.6% | NA | -2.3% |
| “No treatment”b | NA | 32.9% | NA | NA | NA | NA | |
BMD, bone mineral density; NA, not applicable
- a
Estimated as -3.3% and adjusted to 0%
- b
No treatment taken as pre-treatment from the trial
It is important to note that vitamin D plus calcium is associated with a 0% probability of fracture post-treatment in children and young people with cerebral palsy at increased risk of reduced BMD which is questionable. This study included participants who had spastic quadriplegia cerebral palsy who were bedridden and required assisted feeding. Those participants provided a low pre-treatment BMD (0.38) whereas the baseline BMD applied to the population at increased risk of reduced BMD was substantially larger (0.58). The model assumed the same relative treatment effect in this population as in the study population (study pre- vs. post- treatment, 0.38 vs. 0.48; adjusted pre- vs. post-treatment, 0.58 vs. 0.73) but this could potentially over-estimate post-treatment BMD in children and young people at increased risk of reduced BMD if they have “less room for improvement”.
G.9.4. Methods: measurement and valuation of health effects
The quality adjusted life year (QALY) is NICE’s preferred measure of benefit for economic evaluation. This is because it can be seen as a generic measure of health which allows a comparison across treatments which affect different dimensions of health.
The QALY reflects the 2 principle objectives of health care:
- increase longevity;
- increase quality of life.
Estimating a QALY involves placing a quality of life weight on a particular event. This quality weight lies between 0 and 1, where 1 denotes full or ‘perfect health’ and 0 denotes death.
In the model there are the following scenarios to consider when estimating quality of life:
- utility of children and young people with cerebral palsy at increased risk of reduced BMD in the absence of a fracture;
- utility of children and young people with cerebral palsy with proven osteoporosis in the absence of a fracture;
- utility of children and young people with cerebral palsy who require a standing frame in the absence of a fracture;
- utility of children and young people with cerebral palsy at increased risk of reduced BMD who experience a fracture;
- utility of children and young people with cerebral palsy with proven osteoporosis who experience a fracture;
- utility of children and young people with cerebral palsy who require a standing frame who experience a fracture.
A separate systematic search to identify utility values for children and young people with cerebral palsy was not undertaken. Instead, a search was conducted on the Cost-effectiveness analysis (CEA) Registry (using the term “cerebral palsy” in July 2015. This search identified 4 studies with health states relevant to cerebral palsy (Cahill 2011; Obido 2009; Heintz 2008; Carroll 2006). After title and abstract screening only 1 of those studies identified considered people with cerebral palsy, subsequently the full-text of Heintz 2008 was obtained and assessed for inclusion.
Heintz 2008 estimated QALY weights for individuals diagnosed with cerebral palsy based on the utility values reported in the study by Rosenbaum 2007. Consequently, the full-text of Rosenbaum 2007 was retrieved and assessed to inform the utility weights in the model.
Rosenbaum 2007 asked carers to complete the HUI3 – a quality of life survey - on behalf of the person with cerebral palsy they cared for. The resulting score was then transformed into a utility value based on an algorithm using Canadian population values. The utility scores estimated for 192 people with cerebral palsy according to their GMFCS level are presented in Table 42.
Table 42Utility values according to GMFCS level
| GMFCS | Number of people with CP | Utility value | S.E. |
|---|---|---|---|
| Level I | 60 | 0.84 | 0.20 |
| Level II | 33 | 0.50 | 0.31 |
| Level III | 27 | 0.39 | 0.21 |
| Level IV | 46 | 0.16 | 0.26 |
| Level V | 30 | -0.08 | 0.23 |
CP, cerebral palsy; GMFCS, gross motor function classification system; SE, standard error
The methods used to derive utility values within Rosenbaum 2007 are not in line with the NICE reference case which specifies patients to assess their own quality of life using the EQ-5D valued by a representative sample of the UK population. However in the absence of alternative values this study was considered the best available to inform the model.
As can be seen from Table 42 a higher GMFCS level is associated with a lower utility value which reflects a lower quality of life. Based on the inclusion criteria summarised in Table 35, it was assumed children and young people with cerebral palsy in the population at increased risk of reduced BMD would have the greatest functioning ability out of the 3 populations included in the model.
Another search was conducted on the CEA Registry using terms to identify people experiencing a fracture of the leg (or femur), or lower limb (or tibia or fibia). However, the majority of studies retrieved were based on an older population of women and were considered to be irrelevant. This included the submission of evidence undertaken by Amgen in NICE TA204. Amgen used a utility multiplier of 0.70 for a hip fracture and 0.64 for a vertebral fracture in the first year based on a systematic review of the literature.
In light of this, the Committee agreed a utility multiplier of 0.60 would be reasonable for a base case analysis for a fracture of the femur or lower limb in children and young people who were ambulant. However, the Committee noted that a fracture would have less of an impact on their quality of life if they were non-ambulant as this would make less of a difference to their current lifestyle. Consequently, the multiplier was increased to 0.7 for the proven osteoporosis and 0.8 for the postural management populations, respectively. In the model the disutility from a fracture is assumed to last 1 year, over a 5-year time horizon in the third population, this occurs half way through the model in year 3.
To reflect the variability of this estimate, a scenario using a utility multiplier of 0.7 across the populations was undertaken (Section G.9.7.1 and Section G.9.9.2).
The GMFCS levels assigned to each of the populations and the utility in the event of a fracture are presented in Table 43. It is important to note that a population with proven osteoporosis would include some children and young people with cerebral palsy functioning at GMFCS level V, however a negative utility value was considered to be too low, hence GMFCS level IV was used to inform the model.
The Committee noted that a utility value of 0.16 was very low for children and young people with cerebral palsy with proven osteoporosis, or with postural management needs. They believed that if children and young people with cerebral palsy completed the questionnaire themselves their quality of life would provide a higher utility value. Consequently, a scenario using a utility value of 0.39 reported by Rosenbaum 2007 for GMFCS level III was explored as a sensitivity analysis for those 2 populations functioning at GMFCS level IV (Section G.9.7.1 and Section G.9.9.2).
Table 43Utility values assigned to each population
| Population | GMFCS level | Utility value, no fracture | Utility multiplier in the event of a fracture | Utility value, with fracture |
|---|---|---|---|---|
| At increased risk of reduced BMD | II | 0.500 | 0.6 | 0.300 |
| Proven osteoporosis | IV | 0.160 | 0.7 | 0.112 |
| Postural management | IV | 0.160 | 0.8 | 0.128 |
BMD, bone mineral density; GMFCS, gross motor function classification system
G.9.5. Methods: resource and cost use
G.9.5.1. Cost of fracture
The literature was searched to estimate the cost of a fracture, but the populations identified were based largely on post-menopausal women and considered irrelevant. This included the submission of evidence undertaken by Amgen in NICE TA204 who noted vertebral and femur (or upper limb) fracture ICD diagnosis codes were not included in Healthcare Resource Group (HRG) codes relating to a fracture diagnosis. Instead they used International Classification of Diseases (ICD) HRG codes relating to hip traumas as a proxy.
Overall, NHS Reference Costs 2014/15 do not report the cost of a fracture in the femur or the lower limb, but the Committee thought it was reasonable to use the cost of a hip fracture as a proxy in the absence of alternative reliable costing data to reflect the methods used by Amgen. Procedures that related to complications and comorbidities were also preferred as they were considered applicable to a population with cerebral palsy. The Committee stated that major procedures would include a large share of elderly people, for this reason intermediate procedures were used to inform the cost of fracture in children and young people with cerebral palsy.
The currency codes from NHS Reference Costs 2014/15 used to inform the cost of a fracture to the femur in the base case are presented in Table 44.
Table 44Summary of fracture treatment costs included in the model
| Currency description | National average unit cost | Currency code | Average |
|---|---|---|---|
| Intermediate Hip Procedures for Trauma, with CC Score 4+ | £8,735 | HT14A | £7,104 |
| Intermediate Hip Procedures for Trauma, with CC Score 2-3 | £5,473 | HT14B |
CC, complications and comorbidities
To reflect the range of fractures presented in clinical practice a sensitivity analysis (Section G.9.7.1 and Section G.9.9.2) has been conducted using costs for a lower limb fracture considered to be less severe and less costly (NHS Reference Costs 2014/15, HT24D, Intermediate Knee Procedures for Trauma, 18 years and under £2,829).
G.9.6. Cost of non-pharmacological treatments
Purchasing a standing frame, cycling equipment or vibration plate is a capital cost, requiring an up-front payment. There are 2 aspects to capital costs:
- Opportunity cost – this is the money spent on equipment that could have been invested in another venture. This cost is calculated by applying an interest rate on the sum invested in the capital.
- Depreciation cost – the equipment has a certain lifespan and depreciates over time, and will eventually need to be replaced.
The usual practice for economic evaluation is to calculate an ‘annual equivalent cost’. This is calculated by annuitizing the initial capital outlay over the expected life of the equipment. Calculating the equivalent annual cost means making allowance for the differential timing of costs by discounting.
The formula for calculating the equivalent annual cost is:
Where:
- E = equivalent annual cost
- K = purchase price of equipment
- S = resale value
- r = discount (interest) rate
- n = equipment lifespan
- A(n,r) = annuity factor (n years at interest rate r)
Using this formula, a cost per person per annum for use of a standing frame, cycling equipment and vibration plate was calculated to allow for comparison.
It is important to note that the cost of occupational therapists and physiotherapists used to inform the model are based on a band 5 salary, but in some cases bands 6 or 7 may undertake the same tasks, according to the Committee. However, it was agreed that the costs based on band 5 would be reasonable to inform the model.
Use of standing frame as postural management
Each child or young person with cerebral palsy would be provided with their own individualised standing frame. The Committee also noted that some children and young people with cerebral palsy may have 2 standing frames – 1 for use at home and another at their school. However, it was agreed that the cost of 1 standing frame to inform the model would be reasonable.
There are many different types of standing frames available in the UK that vary in price according to the manufacture, model and purpose (upright, prone or standing). Based on this, it would be inappropriate to suggest a “one-price-fits-all” because the equipment would be individualised to the child or young person with cerebral palsy; from a list of manufactures and models provided by the Committee, the upfront capital cost could range from approximately £2,000 to £8,000. Moreover, Jekovec 2000 did not report the specific standing frames used in the study stating that participants used a variety of upright and semi-prone standing frames.
For costing purposes, an upfront capital cost of £4,500 was chosen to represent the cost of the average standing frame in the model. The Committee stated that a person with cerebral palsy would have 2 to 3 standing frames over their childhood and early adult years to match their growth. For this reason, it was assumed that a standing frame can be used for approximately 5 years before it needs to be replaced.
To reflect the range of standing frames available a sensitivity analysis varying the upfront capital cost by ±50% was undertaken (Section 73G.9.7.1 and Section G.9.9.2).
Table 45 below presents the parameters used to calculate the equivalent annual cost.
Table 45Standing frame - annual costs
| Parameter | Value | Source |
|---|---|---|
| K = purchase price of a standing frame (excluding VAT) | £4,500 | Assumption informed by the Committee |
| S = resale value | £0 | Assumption |
| r = discount (interest) rate | 3.5% | NICE reference case |
| n = equipment lifespan | 5 | Assumption informed by the Committee |
| A(n,r) = annuity factor (n years at interest rate r) | 4.67 | Calculated |
| Equivalent annual cost | £963 | Calculated |
| Annual maintenance cost | £36 | Annual review with a community physiotherapist or community occupational therapist, per hour of patient contact, PSSRU 2015 |
| Total annual cost | £999 | Calculated |
NA, not applicable; PSSRU, Personal Social Services Research Unit; VAT, value added tax
In addition to the initial capital outlay, the frame should be reviewed annually, especially with children as the set up would need to be adjusted for growth and changes in the person’s presentation. This would usually be performed by a physiotherapist or occupational therapist. Adding this annual review to the equivalent annual cost results in a total annual cost of £999 per person.
Use of vibration therapy as passive exercise
Purchasing vibration equipment is a capital cost, requiring an up-front payment. Ruck 2010 included in the review used a Vibraflex Home Edition II, but a cost for this particular vibration plate was unable to be sourced. Subsequrntly, a cost of approximately £500 (excluding VAT) was used to inform the model based on the Committee’s experience with vibration equipment. It was also assumed that the equipment can be used for approximately 5 years before it needs to be replaced. Table 46 below presents the parameters used to calculate the equivalent annual cost.
Table 46Vibration equipment - equivalent annual cost
| Parameter | Value | Source |
|---|---|---|
| K = purchase price of a vibration plate (excluding VAT) | £500 | Assumption informed by the Committee |
| S = resale value | £0 | Assumption |
| r = discount (interest) rate | 3.5% | NICE reference case |
| n = equipment lifespan, years | 5 | Assumption informed by the Committee |
| A(n,r) = annuity factor (n years at interest rate r) | 4.67 | Calculated |
| Equivalent annual cost | £107 | Calculated |
VAT, value added tax
If each child or young person with cerebral palsy was provided with their own personal vibration equipment the cost per person per year would equal £107. However, in clinical practice the equipment would be purchased by a school, child development centre or cerebral palsy centre to be used by all of their eligible members with cerebral palsy. In this case a cost per person per annum can be calculated based on the typical use of the equipment per annum. The cost per person will vary depending on the usage of the equipment i.e. the more the equipment is used the lower the cost per person. The formula for calculating the cost per visit is:
Table 47Vibration equipment - cost per visit
| Parameter | Value | Source |
|---|---|---|
| Fixed costs per annum | ||
| E = equivalent annual cost | £107 | Estimated |
| M = annual maintenance | £0 | Assumption informed by the Committee |
| Nv = number of vibration plates per centre | 1 | Assumption informed by the Committee |
| Np = number of CP participants per centre per annum | 50 | Assumption informed by the Committee for a typical centre |
| Total fixed cost per person | £2.14 | Calculated |
| Variable costs per annum | ||
| D = disposables | £0 | Assumption |
| C = cost of health care professional | £18 | Community physiotherapist per 30 minutes of patient contact, PSSRU 2015 |
| Ns = number of sessions per week | 5 | Assumptions informed by the Committee and number undertaken in the trial by Ruck 2010 |
| V = Cost of vibration therapy per annum | £4,682 | Calculated |
| Total cost per week (5 sessions) | £90.04 | Calculated |
CP, cerebal palsy; PSSRU, Personal Social Services Research Unit; VAT, value added tax
As can be seen from Table 47, the cost of the vibration device is negligible compared to the cost of the visit with a physiotherapist. According to the Committee, vibration therapy would need to be used 5 times per week for the benefits of this intervention to be seen with regards to BMD; however, they acknowledged that this could be quite a burden to the child and young person with cerebral palsy and their family or carers.
Based on those assumptions, the cost per year per person based on 5 sessions per week would equal approximately £4,682. To reflect the range of vibration plates available, a sensitivity analysis varying the upfront capital cost by ±50% was undertaken (Section G.9.7.1 and Section G.9.9.2).
As an aside, the Committee noted that vibration therapy can aid exercise programmes to provide benefits beyond BMD that may entail less intensive regimens. Moreover, vibration therapy may be used alongside other interventions to prevent reductions in BMD; however, combined interventions were not identified in the clinical evidence review.
Active exercise programmes
The programmes included in the trials were weight-bearing exercise and home-based virtual cycling. Other forms of active exercise, such as rebound therapy (trampolining), sports or other fitness equipment such as treadmills, were not identified in the clinical evidence review. The cost of these programmes including the cost of equipment would be similar to cycling, but there is no evidence to show equivalent efficacy; hence the model focussed on cycling as the active exercise programme.
To explore the cost-effectiveness of active exercise without the need to purchase equipment, a sensitivity analysis was undertaken with zero equipment cost (Section G.9.7.1 and Section G.9.9.2).
The Committee agreed that weight-bearing exercise and home-based virtual cycling could be performed without supervision from a health care professional at the child or young person’s home or school. The activities would require at least 1 initial visit from a physiotherapist to teach the child or young person with cerebral palsy and their family or carers how to perform the techniques. Thereafter, the physiotherapist would make follow-up visits ideally every 3 months to assess the impact of the programme and modify as necessary. According to the PSSRU each 30 minute visit from a community occupational therapist or physiotherapist would cost approximately £18.
The trials included in the clinical evidence review performed exercise up to 5 days per week. Daily regimens would be ideal for the benefits of the programmes to be realised, but the Committee noted that families would not be able to follow such intensive regimens. The most families would be expected to achieve is 2 to 3 sessions per week as they may have additional programmes to follow. Overall, this could be quite a burden to the child and young person with cerebral palsy and their family or carers, unless it is something that they choose to do, or enjoy.
On the other hand, active exercise programmes could be incorporated into normal school sports or play, which could increase adherence. Table 48 below presents the cost of an active exercise programme that involves cycling. An exercise bike is assumed to cost £200, but over the lifespan of the equipment (5 years) the equivalent annual cost would be £43. Assuming each child or young person with cerebral palsy has their own bike and has input from their physiotherapist 4 times a year, the total cost per annum is approximately £133.
Excluding the cost of a bike, weight bearing activities are assumed to cost £90 per annum based on an equivalent monitoring schedule with a physiotherapist.
Table 48Cost of active exercise programmes
| Intervention | Cost |
|---|---|
| Cycling | |
| Cost of initial physiotherapy session (1 hour) | £36 |
| 3 monthly reviews (30 minutes per visit) | £18 * 3 = £54 |
| Equivalent annual cost | £43 |
| Total cost per person per annum | £133 |
| Weight bearing exercise | |
| Cost of initial physiotherapy session (1 hour) | £36 |
| 3 monthly reviews (30 minutes per visit) | £18 * 3 = £54 |
| Total cost per person per annum | £90 |
G.9.6.1. Supplementation
Acquisition costs
Vitamin D
One study included in the clinical review (Iwasaki 2008) included alfacalcidol as an intervention to prevent reduced BMD. However, this study did not report the dose of alfacalcidol participants received. According to the BNF adults and children over 12 years or with a bodyweight over 20 kg should receive 250 to 500 nanograms daily, whereas children under 20 kg should receive 15 to 30 nanograms/kg (max. 500 nanograms) daily.
Table 49 below presents the acquisition cost of alfacalcidol over the course of 1 year of continued use based on a dose of 500 nanograms daily.
Vitamin D plus calcium acquisition cost
One study included in the clinical review (Jekovec 2000) administered 500 mg elemental calcium and 0.25 µg of calcitrol daily to prevent reduced BMD. However, this study did not report the specific type of elemental calcium participants received.
Elemental calcium refers to the amount of pure calcium there is in the preparation and is independent of the actual compound. The Committee noted that it is important to know how much pure calcium is being prescribed rather than the combined weight of the calcium compound, but advised that the most common elemental calcium prescribed is Cacit-D3 (1 sachet daily) even though this drug is not licensed for use in children under 12 years. Table 50 below presents the cost of calcium supplementation with vitamin D over the course of 1 year of continued use.
Table 50Acquisition cost of vitamin D and calcium (calcitrol)
| Drug | Quantity | Basic price | Unit cost | Cost per year |
|---|---|---|---|---|
| Calcitrol 250 nanogram capsules | 100 | £18.04a | £0.18 | £65.85b |
| Cacit-D3 effervescent granules | 30 | £4.06c | £0.14 | £49.40d |
| Total cost | NA | NA | NA | £115.24 |
NA, not applicable
- a
October 2016 NHS Electronic Drug Tariff
- b
Assume 250 nanograms daily
- c
October 2016 BNF NHS indicative price
- d
Assume 1 sachet daily
Monitoring costs
Children and young people with cerebral palsy who receive vitamin D and/or calcium supplementation would be reviewed every 6 months by their community paediatrician, but this is common to all interventions. For this reason, zero monitoring costs are included in the model for vitamin D and/or calcium supplementation.
Total costs of supplementation
The total annual cost including drug acquisition costs and monitoring cost per person is presented in Table 51.
Table 51Total annual cost of supplementation
| Resource and cost use | Total annual cost |
|---|---|
| Vitamin D only | |
| Drug acquisition cost | £63 |
| Monitoring cost | £0 |
| Total annual cost | £63 |
| Calcium plus vitamin D | |
| Drug acquisition cost | £115 |
| Monitoring cost | £0 |
| Total annual cost | £115 |
G.9.6.2. Bisphosphonates
Acquisition costs
Risedronate plus vitamin D
One study included in the clinical review (Iwasaki 2008) evaluated alfacalcidol (vitamin D) and risedronate as an intervention to prevent reduced BMD. However, this study did not report the dose of alfacalcidol (vitamin D) and risedronate participants received. Subsequently, the Committee advised that Actonel Once a week (35mg) would be the most commonly prescribed risedronate for children and young people with cerebral palsy.
In the trial, participants also received vitamin D (alfacalcidol); to ensure cost-effectiveness is accurately represented in the model, this intervention must include risedronate and vitamin D. It is assumed participants received 500nanograms alfacalcidol daily to reflect the dosages reported in the BNF and the vitamin D only intervention (Section G.9.6.1). The total cost of these drugs is presented in Table 52.
Table 52Acquisition cost of risedronate and vitamin D (alfacalcidol)
| Drug | Quantity | Basic price | Unit cost | Cost per year |
|---|---|---|---|---|
| Risedronate 35mg | 4 | £0.89a | £0.22 | £11.57b |
| Vitamin D, alfacalcidol, 500 nanogram capsule | 30 | £5.18a | £0.17 | £63.02c |
| Total cost | NA | NA | NA | £74.59 |
NA, not applicable
- a
October 2016 NHS Electronic Drug Tariff
- b
Assume 1 35mg tablet per week
- c
Assume 1 capsule daily
Unlike pamidronate disodium (below), risedronate is administered orally at home; hence there are no administration costs.
Pamidronate disodium
One study included in the clinical review (Henderson 2002) included pamidronate disodium as an intervention to prevent reduced BMD. This drug was administered as an inpatient procedure intravenously over 3 to 4 hours, for 3 consecutive days, repeated at 3-month intervals. Each daily dose was 1 mg pamidronate disodium /kg body weight but not <15 mg or >30 mg.
According to the BNF, pamidronate disodium is for specialist use only and not licensed for use in children. Despite this, the Committee advised that in clinical practice today, pamidronate disodium would be administered as a day case procedure by a specialist nurse over 2 days.
Costing data on pamidronate disodium administration was sought, subsequently NICE TA265 was identified that included pamidronate disodium as an intervention. To estimate the administration costs associated with pamidronate disodium, the manufacturer commissioned a micro-costing study. This study was undertaken in the UK among 80 oncology nurses and 20 oncology pharmacists, the administration costs utilised in their model, taken from the Aberdeen Assessment Group are summarised in Table 53.
Table 53Administration costs incurred by pamidronate disodium taken from TA265
| Administration | Costa |
|---|---|
| Staff time | £138.49 |
| Monitoring cost | £1.41 |
| Consumables | £7.24 |
| Capital costs | £1.84 |
| Total | £148.98 |
- a
Cost year 2011
The costs reported by the Aberdeen Assessment Group were subsequently inflated from 2011 prices using the Hospital and Community Health Services Index (HCHS) to 2014/15 prices to inform the model. In addition to administration costs, children and young people with cerebral palsy would be admitted to hospital incurring the cost of an inpatient stay.
The Committee also noted that a dose of 1.5mg/kg per day for 2 days every 3 months in children over 3 years of age would be a reasonable assumption to inform the model according to their protocols.
Table 54 below presents the cost of pamidronate disodium based on a weight of 37kg to reflect the ages of participants (11 years) included in the clinical evidence review.
Table 54Cost of pamidronate disodium
| Resource | Cost per day | Cost per 2 day attendance | Annual costa | Source |
|---|---|---|---|---|
| Drug acquisition | £115.25 | £230.50 | £922.00 | £115.25 per 6 mg/mL 10-mL vial (BNF, October 2016) 37kg bodyweight requires 55.5 mg (1 vial) |
| Administration | £154.57 | £309.14 | £1,236.56 | NICE TA265 (Table 53) inflated by 1.0375 to 2014/15 prices based on the HCSC (293.1 [2015 PPI] / 282.5 [2011 PPI]) |
| Inpatient stay | £1,472.73 | £1,472.73b | £4,418.18 | NHS Reference Costs 2014/15, Paediatric, Examination, Follow-Up, Special Screening or Other Admissions, with CC Score 1-3, PX57B |
BNF, British National Formulary; CC, complications and comorbidities; HCSC, Hospital and Community Health Services; NICE, National Institute of Health and Care Excellence; PPI, pay and prices index; TA, technology appraisal
- (a)
administered over 2 days, repeated after 3 months
- (b)
assumed to cover the inpatient stay over 2 days
Monitoring costs
Children and young people with cerebral palsy would be reviewed annually by a specialist paediatrician who would perform bone, blood, liver, renal, and vitamin D investigations every 6 months and a DEXA scan every 12 months. This would be in addition to the standard monitoring schedule in place for other interventions. The total monitoring cost per year is presented in Table 55.
Table 55Bisphosphate monitoring costs
| Resource use | Cost | Source |
|---|---|---|
| Dual energy X-ray absorptiometry (DEXA) scan | £60.65 | NHS Reference Costs 2014/15, DIAGIMDA, RD50Z |
| Tertiary/specialist paediatrician | 2x £203 | NHS Reference Costs 2014/15, WF01A NonAdmitted Face to Face Attendance, Follow-up, Paediatric Endocrinology 252 |
| Bone, blood, liver, renal, and vitamin D investigations | 2x £30 | Assumption informed by the Committee |
| Total cost per annum | £526.65 | Calculated |
Total cost of bisphosphonates
The total annual cost per person incorporating drug acquisition costs, administration costs (pamidronate disodium) and monitoring costs are presented in Table 56.
Table 56Total annual cost of bisphosphonates
| Resource and cost use | Total annual cost |
|---|---|
| Risedronate plus vitamin D | |
| Drug acquisition cost | £75 |
| Administration cost | £0 |
| Monitoring cost | £527 |
| Total annual cost | £601 |
| Pamidronate disodium | |
| Drug acquisition cost | £922 |
| Administration cost (including inpatient stay) | £5,655 |
| Monitoring cost | £527 |
| Total annual cost | £7,103 |
G.9.6.3. “No treatment”
The Committee noted that “no treatment” would not incur zero cost in clinical practice as children and young people with cerebral palsy would undergo bone, blood, liver, renal, and vitamin D investigations at least every 12 months. Moreover, these investigations would not be common practice across all the comparators under consideration. The cost of the individual tests would be relatively inexpensive (NHS Reference Costs 2014/15, Pathology services, DAPS05, Haematology, £3). Including staff time, the Committee advised a cost of £30 would be reasonable to inform the model.
G.9.6.4. Summary of treatment costs
Table 57 below presents the total annual costs included in the model for each intervention.
Table 57Summary of intervention costs included in the model
| Population | Interventions | Total annual cost |
|---|---|---|
| At increased risk of reduced BMD | Active exercise (cycling) | £133 |
| Weight-bearing exercise | £90 | |
| Vitamin D | £63 | |
| Vitamin D plus calcium | £115 | |
| Vibration therapy | £4,682 | |
| “No treatment” | £30 | |
| Proven osteoporosis | Pamidronate disodium | £7,103 |
| Vitamin D plus calcium | £115 | |
| Risedronate plus vitamin D | £601 | |
| Vitamin D | £63 | |
| Postural management | Standing frame | £999 |
| “No treatment” | £30 |
G.9.7. Methods: sensitivity analysis
G.9.7.1. Deterministic sensitivity analysis
A series of scenario analyses were undertaken in order to test how sensitive the results are to uncertainty in individual parameters. Parameters varied in the scenario analysis were chosen on the basis of uncertainty in their estimation or the potential impact that they had on the results. The values varied, along with their rationale are shown in Table 58.
Table 58Description of sensitivity analysis
| Scenario analysis, parameter(s) to be changed | Default parameter value | Value tested | Rationale |
|---|---|---|---|
| 1. Utility multiplier | Without osteoporosis, 0.6; postural management, 0.8 | 0.7 | There is insufficient evidence to accurately estimate the disutility from a fracture in children and young people with cerebral palsy. Moreover the type and severity of fracture can vary, for example, a nonambulant person who relies on their hand may find this more damaging to their quality of life than a fracture to the lower limb. |
| 2. Cost of fracture | £7,104 | £2,829 | There is insufficient evidence to accurately estimate the cost of a fracture in children and young people with cerebral palsy. Moreover the type and severity of fracture can vary. The base case reflects a severe fracture to the femur (hip); hence a fracture to the lower limb (knee) considered to be less costly was explored. |
| 3. Utility value (no fracture) increased for GMFCS level IV | 0.16 | 0.39 | The Committee believed a utility value of 0.16 was too low for GMFCS level IV. Standard errors reported by Rosenbaum 2007 were also quite large demonstrating the uncertainty around the mean value. |
| 4. Iwasaki 2008 regression equation for vitamin D and risedronate | As described in Table 66 | Regression equation reported by Iwasaki 2008: Vitamin D, first line, 0.69; Vitamin D, proven osteoporosis, 0.36; Risedronate plus vitamin D, 0.39. Described further in Table 66 in the Appendix. | The regression equation is dependent on the pre-treatment BMD, this can be inputted using the common baseline BMD which may provide a different post-treatment BMD to those estimated in the base case using the methods described in Table 64 |
| 5. Standing frame upfront capital cost | £4,500 | 50% increase and decrease | A range of manufacturers and models are available that vary in price. |
| 6. Vibration plate upfront capital cost | £500 | 50% increase and decrease | A range of manufacturers and models are available that vary in price. |
| 7. Zero active exercise equipment cost | £200 | £0 | Active exercise may not involve equipment |
BMD, bone mineral density; GMFCS, Gross Motor Function Classification System
G.9.7.2. Probabilistic sensitivity analysis (PSA)
PSA was conducted in the model to take account of the simultaneous effect of uncertainty relating to model parameter values. Key parameters were varied by sampling from probability distributions.
The model was run for 1,000 simulations to generate estimates of total costs and QALYs for each treatment arm by varying probabilities, costs and utilities simultaneously. Those simulations are presented on cost-effectiveness planes with a willingness-to-pay (WTP) threshold of £20,000 per QALY and over several thresholds using cost-effectiveness acceptability curves (CEACs). The model structure and model settings were kept constant. Drug costs are known with certainty hence only the total treatment cost has been varied which includes monitoring, and/or the purchase of equipment.
A beta probability distributions was employed for probabilities and utilities, whilst a gamma probability distribution was employed for costs. It is important to note that utilities are assumed to be bound by 0 and 1; hence values worse than death are not possible, consequently the probabilistic values are positively skewed towards 0 given the low GMFCS levels under consideration. A starting point for unknown data was to assume the value of the standard deviation was 20% of the expected input parameter mean – such conservative methods are often used by manufacturers in Technology Appraisal submissions (such as NICE TA354 and NICE TA327) when the distribution of the data is not available. PSA parameters are provided in Table 67.
If the underlying probability distribution is unknown then PSA may be less informative in quantifying the uncertainty arising from model inputs. However, undertaking PSA was considered to be useful to the Committee to illustrate the possible simulations that could result from the assumptions made in the model.
G.9.8. Model validation
Validation was assessed using 2 primary criteria, internal (verification) and external consistency (validation). Internal validity addresses whether the model has been implemented correctly, and examines the extent to which the mathematical calculations are performed correctly and are consistent with the model’s specifications. Face validation helps to ensure a model is constructed and used in accord with the best available evidence. This process enhances credibility with experts and increases acceptance of results.
Internal validity was assessed by the primary modeller, and a second health economist who also completed the Philips Checklist (PSA, probabilistic sensitivity analysis; SD, standard deviation Table 68). The following areas of the model were checked:
- plausibility and accuracy of inputs and assumptions;
- programming of formulae and macros;
- efficacy and cost parameters were altered to check whether results changed in the expected direction;
- sensitivity analyses using zero and extreme values were undertaken to check whether results changed as expected;
- input parameters in all arms of the model were set at the same value to check whether outputs (costs and QALYs) in all arms became equal.
External consistency was assessed by assessing the face validity of the model, and comparing the results of the analysis against the clinical evidence review and other published data (cross validation). It was also assessed with members of the Committee whether the setting, population, interventions, outcomes, assumptions, and time horizons correspond to those of decision problem.
G.9.9. Results
If there is strong evidence that an intervention dominates the alternatives (that is, it is both more effective and less expensive), it should normally be recommended. However, if one intervention is more effective but also more expensive than another, then the incremental cost-effectiveness ratio (ICER) should be considered as a measure of whether the intervention would represent an efficient use of resources for the NHS. Here the ICER is the difference in the mean costs (incremental costs) divided by the differences in QALYs gained (incremental QALYs). It is important to note that these estimates of cost-effectiveness are highly uncertain due to the assumptions used to convert the intermediate outcome (BMD) into a final outcome (risk of fracture), therefore the cost-utility analysis should be interpreted with caution.
NICE does not formally have a threshold for cost-effectiveness, but an ICER below £20,000 would generally be considered cost-effective, whereas an ICER above £30,000 would generally not be considered cost-effective without additional justifications.
G.9.9.1. Base case
Table 59 below presents the total costs and total QALYs associated with each intervention in the model. It is important to note that the total costs incorporate the cost of treatment to prevent reduced BMD (Table 57) plus the expected cost of fracture treatment (Table 44).
For example, if 1 child or young person with cerebral palsy enters the population at increased risk of reduced BMD and receives vitamin D as an intervention the cost of treatment is £53. They have a 10.8% probability of receiving fracture treatment at a cost of £7,104 which results in an expected fracture cost of £765 (10.8% x £7,104). As a result, the total expected cost for that person over 1 year is £828 (£63 + £765).
The same principle of expected values are used to calculate the total QALYs. Our child or young person with cerebral palsy in the first line population receiving vitamin D will experience a fracture with a probability of 10.8% associated with a utility of 0.3 or not experience a fracture a probability of 89.2% associated with a utility of 0.5. Therefore, over 1 year that person will expect to accrue a total of 0.4785 QALYs (0.108 × 0.3 + 0.892 × 0.5).
Table 59Total costs and total QALYs
| Population | Intervention | Total cost | Total QALYs |
|---|---|---|---|
| At increased risk of reduced BMD | Active exercise (cycling) | Lumbar spine: £1,014 F1: £905 | Lumbar spine: 0.4752 F1: 0.4783 |
| Weight-bearing exercise | F1: £806 | F1: 0.4798 | |
| Vitamin D | F1: £828 | F1: 0.4785 | |
| Vitamin D plus calcium | Lumbar spine: £115 | Lumbar spine: 0.5000 | |
| Vibration therapy | Lumbar spine: £5,451 F1: £5,403 | Lumbar spine: 0.4784 F1: 0.4797 | |
| “No treatment” | Lumbar spine: £889 F1: £830 | Lumbar spine: 0.4758 F1: 0.4775 | |
| Proven osteoporosis | Pamidronate disodium | Lumbar spine: £9,142 F1: £8,393 | Lumbar spine: 0.1462 F1: 0.1513 |
| Vitamin D plus calcium | Lumbar spine: £2,364 | Lumbar spine: 0.1448 | |
| Vitamin D plus risedronate | F1: £2,536 | F1: 0.1469 | |
| Vitamin D | F1: £2,038 | F1: 0.1467 | |
| Postural management | Standing frame | Lumbar spine: £7,165a | Lumbar spine: 0.7190a |
| “No treatment” | Lumbar spine: £2,475a | Lumbar spine: 0.7183a |
BMD, bone mineral density; QALYs, quality-adjusted life years
- (a)
Costs and benefits discounted over 5 years at 3.5%/year
It is important to note that the difference in total QALYs across the treatments is small and can lead to substantial changes in the resulting ICER.
Only pair-wise comparisons were estimated in the model because there is insufficient clinical data to present a fully incremental comparison for one BMD site; consequently the site of BMD is a user input in the model when more than one site is available for each treatment. Furthermore, interventions are not mutually exclusive in the population at increased risk of reduced BMD, and there is no evidence on their combined effect. Consequently, there are a substantial number of comparisons that can be made for the populations at increased risk of reduced BMD and with proven osteoporosis. For pragmatic reasons the Committee was asked to prioritise their comparisons of interest in those populations:
- Population at increased risk of reduced BMD:
- vitamin D plus calcium vs. “no treatment”
- aerobic exercise (cycling) vs. “no treatment”
- Proven osteoporosis population:
- risedronate (plus vitamin D) vs. pamidronate disodium
For those comparisons, cost-effectiveness planes (CE planes) are presented in addition to the ICER. Sensitivity analysis was also conducted on those comparisons (Section G.9.7 and Section G.9.9.2).
Site of fracture
For any given Z-score, the lumbar spine reported a higher probability of fracture than the distal femur (F1). When the Z-score gets bigger (more negative) the difference in probability of fracture estimated between the 2 sites increases. If this difference is large enough, the resulting ICER can change substantially when a lumbar spine site is compared to a F1 site.
When the probability of fracture increases, the expected QALYs are reduced and the expected cost of fracture treatment is increased. Consequently, a treatment that was dominant (less expensive and more effective) or had a positive ICER (more expensive and more effective) under a F1 measure could become a less expensive and less effective, or dominated (more expensive and less effective) under a lumbar spine measure if the lumbar spine is not associated with a lower (less negative) Z-score.
Because interventions with an F1 measure may be considered favourable compared to those with only a lumbar spine measure. Therefore, comparisons using equivalent sites are preferable to comparisons using different sites, when possible.
Population at increased risk of reduced BMD
The interventions under consideration in this population are not mutually exclusive; however, combined interventions were not identified in the clinical evidence review. Only comparisons against “no treatment” are discussed and presented here (Table 60). All remaining comparisons estimated by the model are reported in in Table 61.
Table 60Population at increased risk of reduced BMD, base case results (ICER)
| Intervention ▼vs. ▶ | “No treatment” | ||
|---|---|---|---|
| F1 | Lumbar | ||
| Active exercise (cycling) | F1 | £95,041 | £6,261 |
| Lumbar | Dominated a | Dominated a | |
| Weight-bearing exercise | F1 | Dominant b | Dominant b |
| Lumbar | NC | NC | |
| Vitamin D | F1 | Dominant c | Dominant c |
| Lumbar | NC | NC | |
| Vitamin D plus calcium | F1 | NC | NC |
| Lumbar | Dominant d | Dominant d | |
| Vibration therapy | F1 | £2,044,947 | £1,154,538 |
| Lumbar | £5,288,632 | £1,791,107 | |
ICER, incremental cost-effectiveness ratio; NC, not calculable
- (a)
Cycling more expensive and less effective than “no treatment”
- (b)
Weights less expensive and more effective than “no treatment”
- (c)
Vitamin D less expensive and more effective than “no treatment”
- (d)
Vitamin D plus calcium less expensive and more effective than “no treatment”
Intervention: exercise (cycling and weight-beating)
When the effectiveness of cycling is based on the lumbar spine site it is dominated (more expensive and less effective) by “no treatment”. However, when the effectiveness of cycling is based on the F1 site, cycling becomes more effective than “no treatment”. As a result, there are different conclusions according to the site of BMD used for “no treatment”. When F1 sites are compared, cycling would not be considered cost-effective under NICE’s advisory cost-effective threshold. Conversely, cycling would be considered cost-effective when compared to the lumbar site for “no treatment”. As stated previously, the results based on different BMD sites should be interpreted with caution. Figure 4 below presents the cost-effectiveness planes for cycling vs. “no treatment” for all BMD site comparisons.
Weight-bearing exercise would be considered cost-effective to limit reductions in BMD as it dominates (less expensive and more effective) “no treatment”.
Both weight-bearing exercise and cycling are active exercise programmes with negligible difference in their treatment costs. However, their difference in clinical effectiveness is evident as the risk of fracture under cycling is higher than weight-bearing exercise (lumbar, 12.4%; F1, 10.9% vs. F1, 10.1%), but with the caveat that fracture risks are point estimates with some underlying uncertainty as to their true value. From these results, exercise that aims to improve muscle tone from weight-bearing activities would be cost-effective relative to aerobic exercise that improves cardiovascular ability.
Intervention: vitamin D
Vitamin D would be considered cost-effective to limit reductions in BMD as it is dominates (less expensive and more effective) “no treatment”.
Intervention: vitamin D plus calcium
Vitamin D plus calcium dominates (less expensive and more effective) “no treatment”. However, it is important to note that this intervention is assumed to have a zero risk of fracture post-treatment in the model (Section G.9.3.5). Figure 5 below presents the cost-effectiveness planes for cycling vs. “no treatment” for all BMD site comparisons
Intervention: vibration therapy
Vibration therapy would not be considered cost-effective to limit reductions in BMD as it is has an ICER substantially greater than NICE’s advisory cost-effective threshold. This is driven by the high treatment cost associated with vibration therapy, which cannot be offset by larger gains in clinical effectiveness.
Summary
Overall weight-bearing active exercise, vitamin D, or vitamin D plus calcium would be considered cost-effective interventions to limit reductions in BMD in a population of children and young people with cerebral palsy at increased risk of reduced BMD compared to “no treatment” based on the results presented in Table 60. On the other hand, cycling and vibration therapy may not be considered cost-effective compared to “no treatment”.
Children and young people with cerebral palsy with proven osteoporosis
Intervention: vitamin D
Vitamin D would be considered cost-effective, but whether this is a decision of disinvestment (less effective and less expensive) or dominance depends on the comparators site of BMD. When compared to F1 measures i.e. risedronate plus vitamin D or pamidronate disodium, vitamin D is less expensive and less effective. In other words, pamidronate disodium and risedronate plus vitamin D have ICERs above NICE’s advisory cost-effective threshold and neither would not be considered cost-effective relative to vitamin D.
Conversely, when compared to lumbar spine measures i.e. calcium plus vitamin D or pamidronate disodium, vitamin D is less expensive and more effective (dominant). As stated previously, for any given Z-score the lumbar spine reports a higher probability of fracture than the distal femur (F1); hence comparing F1 measures against lumbar spine measures could favour the former intervention. Overall, regardless of the site of BMD vitamin D always produces the lowest total cost.
Intervention: risedronate plus vitamin D
Risedronate plus vitamin D would not be considered cost-effective under NICE’s cost-effective advisory threshold when compared to vitamin D or vitamin D plus calcium.
Risedronate plus vitamin D would be considered cost-effective relative to pamidronate disodium. When F1 measures are compared, pamidronate disodium is more expensive and more effective than risedronate plus vitamin D, but the ICER is substantially above NICE’s advisory cost-effective threshold, hence pamidronate disodium would not be considered cost-effective. When risedronate plus vitamin D is compared to pamidronate disodium using a lumbar spine site, risedronate plus vitamin D is less expensive and more effective than pamidronate disodium, hence pamidronate disodium is dominated by risedronate plus vitamin D. Figure 6 below presents the cost-effectiveness plane for pamidronate disodium compared to risedronate plus vitamin D.
Intervention: calcium plus vitamin D
Calcium plus vitamin D is dominated (more expensive and less effective) by vitamin D. However, calcium plus vitamin D is a lot cheaper and slightly less effective than pamidronate disodium and risedronate plus vitamin D leading to a decision of disinvestment (less expensive and less effective) with substantial cost savings per QALY loss. In other words, pamidronate disodium and risedronate plus vitamin D have ICERs above NICE’s advisory cost-effective threshold and neither would not be considered cost-effective relative to calcium plus vitamin D.
Intervention: pamidronate disodium
Pamidronate disodium would not be considered cost-effective relative to any of the interventions included in the model as it is either dominated or substantially above NICE’s advisory cost-effective threshold.
Table 61Proven osteoporosis base case results (ICER) for all comparisons
| Intervention | Vitamin D | Risedronate + vitamin D | Calcium + vitamin D | Pamidronate disodium | |||||
|---|---|---|---|---|---|---|---|---|---|
| F1 | Lumbar | F1 | Lumbar | F1 | Lumbar | F1 | Lumbar | ||
| Vitamin D | F1 | - | £1,799,501 (SW)a | NC | NC | Dominant b | £1,371,205 (SW) c | Dominant d | |
| Lumbar | NC | NC | NC | NC | NC | NC | |||
| Risedronate plus vitamin D | F1 | £1,799,501 (NE) | NC | - | NC | £81,047 (NE) | £1,344,044 (SW) e | Dominant f | |
| Lumbar | NC | NC | NC | NC | NC | NC | |||
| Calcium plus vitamin D | F1 | NC | NC | NC | NC | - | NC | NC | |
| Lumbar | Dominated g | NC | £81,047 (SW) h | NC | £930,466 (SW) i | £4,782,071 (SW) i | |||
| Pamidronate disodium | F1 | £1,371,205 (NE) | NC | £1,344,044 (NE) | NC | NC | £930,466 (NE) | - | |
| Lumbar | NC | NC | Dominated j | NC | NC | £4,782,071 (NE) | |||
South-west ICERs represent the costs saved per QALY loss
NC, not calculable; NE, north-east quadrant on the cost-effectiveness plane (more expensive and more effective than the comparator); SW, south-west quadrant on the cost-effectiveness plane (less expensive and less effective than the comparator)
- (a)
vitamin D less expensive and less effective than risedronate plus vitamin D
- (b)
vitamin D less expensive and more effective than calcium plus vitamin D
- (c)
vitamin D less expensive and less effective than pamidronate
- (d)
vitamin D less expensive and more effective than pamidronate
- (e)
risedronate plus vitamin D less expensive and less effective than pamidronate
- (f)
risedronate plus vitamin D less expensive and more effective than pamidronate
- (g)
calcium plus vitamin D more expensive and less effective than vitamin D
- (h)
calcium plus vitamin D less expensive and less effective than risedronate plus vitamin D
- (i)
calcium plus vitamin D less expensive and less effective than pamidronate
- (j)
pamidronate more expensive and less effective than risedronate plus vitamin D
Standing frame
Caulton 2004 took BMD measures from the vertebrae and proximal tibia, however for reasons described in Section G.9.3.3 only the vertebral site could be included in the model from the data they reported.
They found a 6% mean increase in vertebral vTBMD in the intervention group; whereas the proximal tibial vTBMD in the intervention group showed a change of −0.85 mg/cm3 compared to the control group (95% CI −16.83 to 15.13; p = 0.92). Overall, these results suggested that a longer period of standing leads to a significant increase in vertebral but not proximal tibial vTBMD in non-ambulant cerebral palsy children, demonstrating that different BMD sites can lead to different conclusions.
The standing frame would not be considered cost-effective to prevent reduced BMD based on the vertebral site as the ICER is substantially higher than NICE’s advisory cost-effective threshold when compared to “no treatment” (Table 62). This combined with their findings that there were no significant difference pre- and post- intervention on the proximal tibial vTBMD reiterates that the standing frame should not be recommended to prevent reduced BMD. However, it is important to note that the normal standing duration has been used as a proxy for “no treatment” which may underestimate the incremental effectiveness of the standing frame. Figure 7 below presents the cost-effectiveness plane.
Table 62Standing frame results
| Treatment | Total cost | Total QALYs | Inc. cost | Inc. QALYs | ICER |
|---|---|---|---|---|---|
| “No treatment” | £2,475 | 0.7183 | - | - | - |
| Standing frame | £7,165 | 0.7190 | £4,691 | 0.0007 | £6,896,073 |
ICER, incremental cost-effectiveness ratio; QALYs, quality-adjusted life years
Costs and benefits discounted at 3.5%/year over a 5-year time horizon
G.9.9.2. Deterministic sensitivity analysis
Comparisons of interest in the population at increased risk of reduced BMD are limited to vitamin D plus calcium, cycling and “no treatment” and in the proven osteoporosis population risedronate plus vitamin D vs. pamidronate disodium, unless otherwise stated. Table 63 presents the resulting ICERs for these comparisons.
Table 63Sensitivity analysis results
| Scenario | Comparison | Base case ICER | Scenario ICER |
|---|---|---|---|
| 1. Multiplier 0.70 for all populations | Vitamin D plus calcium (lumbar spine) vs. no treatment (lumbar spine) | Vitamin D plus calcium dominates no treatment | Vitamin D plus calcium dominates no treatment |
| Vitamin D plus calcium (lumbar spine) vs. no treatment (F1) | Vitamin D plus calcium dominates no treatment | Vitamin D plus calcium dominates no treatment | |
| Cycling (lumbar spine) vs. no treatment (lumbar spine) | Cycling dominated by no treatment | Cycling dominated by no treatment | |
| Cycling (F1) vs. no treatment (F1) | £95,041 (NE) | £126,721 (NE) | |
| Cycling (lumbar spine) vs. no treatment (F1) | Cycling dominated by no treatment | Cycling dominated by no treatment | |
| Cycling (F1) vs. no treatment (lumbar spine) | £6,261 (NE) | £8,348 (NE) | |
| Standing frame vs. no treatment | £6,896,073 (NE)a | £4,597,382 (NE)a | |
| 2. Cost of fracture reduced from £7,104 (femur) to £2,829 (knee) | Vitamin D plus calcium (lumbar spine) vs. no treatment (lumbar spine) | Vitamin D plus calcium dominates no treatment | Vitamin D plus calcium dominates no treatment |
| Vitamin D plus calcium (lumbar spine) vs. no treatment (F1) | Vitamin D plus calcium dominates no treatment | Vitamin D plus calcium dominates no treatment | |
| Cycling (lumbar spine) vs. no treatment (lumbar spine) | Cycling dominated by no treatment | Cycling dominated by no treatment | |
| Cycling (F1) vs. no treatment (F1) | £95,041 (NE) | £116,416 (NE) | |
| Cycling (lumbar spine) vs. no treatment (F1) | Cycling dominated by no treatment | Cycling dominated by no treatment | |
| Cycling (F1) vs. no treatment (lumbar spine) | £6,261 (NE) | £27,636 (NE) | |
| Risedronate plus vitamin D (F1) vs. pamidronate (F1) | £1,344,044 (SW)b | £1,433,106 (SW)b | |
| Risedronate plus vitamin D (F1) vs. pamidronate (lumbar spine) | Risedronate plus vitamin D dominates pamidronate | Risedronate plus vitamin D dominates pamidronate | |
| Standing frame vs. no treatment | £6896,073 (NE)a | £7,044,191 (NE)a | |
| 3. Utility value (no fracture) increased from 0.16 to 0.39 | Risedronate plus vitamin D (F1) vs. pamidronate (F1) | £1,344,044 (SW)b | £551,403 (SW)b |
| Risedronate plus vitamin D (F1) vs. pamidronate (lumbar spine) | Risedronate plus vitamin D dominates pamidronate | Risedronate plus vitamin D dominates pamidronate | |
| Standing frame vs. no treatment | £6,896,073 (NE) | £2,829,158 (NE) | |
| 4. Iwasaki 2008 regression equation for vitamin D and risedronate | Vitamin D (F1) vs. cycling (F1) | Cycling dominated by vitamin D | Vitamin D dominated by cycling |
| Vitamin D (F1) vs. cycling (lumbar spine) | Cycling dominated by vitamin D | £38,434 (SW)b | |
| Vitamin D (F1) vs. weights (F1) | Vitamin D dominated by weights | Vitamin D dominated by weights | |
| Vitamin D (F1) vs. vitamin D plus calcium (lumbar spine) | Vitamin D dominated by calcium plus vitamin D | Vitamin D dominated by calcium plus vitamin D | |
| Vitamin D (F1) vs. vibration therapy (F1) | £3,649,199 (SW) c | £821,016 (SW) d | |
| Vitamin D (F1) vs. vibration therapy (lumbar spine) | Vitamin D dominates vibration therapy | £1,111,051 (SW) d | |
| Vitamin D (F1) vs. no treatment (F1) | £4,338 (NE) | Vitamin D dominated by no treatment | |
| Vitamin D (F1) vs. no treatment (lumbar spine) | Vitamin D dominates no treatment | Vitamin D dominated by no treatment | |
| Risedronate plus vitamin D (F1) vs. pamidronate (F1) | £1,344,044 (SW)b | £1,422,405 (SW) b | |
| Risedronate plus vitamin D (F1) vs. pamidronate (lumbar spine) | Risedronate plus vitamin D dominates pamidronate | Risedronate plus vitamin D dominates pamidronate | |
| Risedronate plus vitamin D (F1) vs. vitamin D (F1) | £1,799,501 (NE) | £808,685 (NE) | |
| Risedronate plus vitamin D (F1) vs. calcium plus vitamin D (lumbar spine) | £81,047 (NE) | £59,756 (NE) | |
| Vitamin D (F1) vs. calcium plus vitamin D (lumbar spine) | Vitamin D dominates calcium plus vitamin D | Vitamin D dominates calcium plus vitamin D | |
| 5a. Standing frame upfront capital cost increased by 50% | Standing frame vs. no treatment | £6896,073 (NE)a | £10,435,178 (NE)a |
| 5b. Standing frame upfront capital cost reduced by 50% | Standing frame vs. no treatment | £6,896,073 (NE)a | £3,356,968 (NE)a |
| 6a. Vibration equipment increased by 50% | Increasing the cost of vibration equipment increase the incremental cost further, consequently vibration therapy is less cost-effective compared the base case against all treatments | ||
| 6b. Vibration equipment reduced by 50% | Vibration therapy vs. cycling | ICER ranges from £52,606,691 to £969,648 for the possible combination of BMD sites | ICER ranges from £52,594,310 to £969,412 for the possible combination of BMD sites |
| Vibration therapy vs. weights | Vibration therapy dominated by weights for each combination of BMD sites | Vibration therapy dominated by weights for each combination of BMD sites | |
| Vibration therapy vs. vitamin D | F1 vs. F1, £3,649,199 (NE); Lumbar spine vs. F1, dominated by vitamin D | F1 vs. F1, £3,648,345 (NE); Lumbar spine vs. F1, dominated by vitamin D | |
| Vibration therapy vs. vitamin D plus calcium | Vibration therapy dominated by vitamin D plus calcium | Vibration therapy dominated by vitamin D plus calcium | |
| Vibration therapy vs. no treatment | ICER ranges from £2,099,161 to £9,615,694 for the possible combinations of BMD sites | ICER ranges from £1,154,265 to £5,287,407 for the possible combinations of BMD sites | |
| 7. Zero active exercise equipment cost | Cycling (lumbar spine) vs. no treatment (lumbar spine) | Cycling dominated by no treatment | Cycling dominated by no treatment |
| Cycling (F1) vs. no treatment (F1) | £95,041 (NE) | £40,684 (NE) | |
| Cycling (lumbar spine) vs. no treatment (F1) | Cycling dominated by no treatment | Cycling dominated by no treatment | |
| Cycling (F1) vs. no treatment (lumbar spine) | £6,261 (NE) | No treatment dominated by cycling | |
ICER, incremental cost-effectiveness ratio; QALYs, quality-adjusted life years; NE, north-east quadrant on the cost-effectiveness plane (more expensive and more effective than the comparator); SW, south-west quadrant on the cost-effectiveness plane (less expensive and less effective than the comparator).
- (a)
Costs and benefits discounted at 3.5%/year over a 5-year time horizon
- (b)
Risedronate plus vitamin D less expensive and less effective than pamidronate
- (c)
Vitamin D less expensive and less effective than cycling
- (d)
Vitamin D less expensive and less effective than vibration therapy
Scenario 1. Utility multiplier 0.70
Reducing the disutility from a fracture in the population at increased risk of reduced BMD favours the less effective treatment and decrease the incremental QALYs between 2 interventions increasing the ICER, but this scenario does not change the resulting decision for any of the comparisons.
Increasing the disutility from a fracture in the population who require postural management favours the more effective treatment (standing frame) and increases the incremental QALYs between 2 interventions, but this scenario does not change the resulting decision as the ICER is still above NICE’s cost-effective threshold.
Scenario 2. Cost of fracture
Reducing the cost of a fracture favours the less effective treatment and/or the more expensive treatment, but total costs will reduce for both treatments. Other things being equal, reducing the cost of fractures will tend to reduce the cost-effectiveness of the comparator which has the lowest probability of fracture.
This scenario increases the incremental cost between 2 treatments resulting in a higher ICER. For cycling (F1) vs. “no treatment” (lumbar) this increases the ICER from £6,261 (below NICE’s threshold) to £27,636 (close to NICE’s upper threshold of £30,000 per QALY). For all remaining comparisons, this scenario does not impact the decision.
However, for vitamin D plus calcium the total cost is unchanged due to a zero risk of fracture. Consequently, the total cost reduces only for “no treatment” reducing the incremental costs. Despite this, the resulting decision is unchanged as vitamin D plus calcium dominates “no treatment” in this scenario and in the base case.
Scenario 3. Utility value (no fracture) increased for GMFCS level IV
Increasing the utility value in the absence of a fracture favours the more effective treatment because greater QALY gains can be achieved. Consequently, the incremental QALYs increase, reducing the ICER; however, the magnitude of this reduction is not sufficiently large enough to change the resulting decision.
Scenario 4. Regression equation for vitamin D and risedronate
Using the regression equation reported by Iwasaki 2008 increases the risk of fracture for vitamin D in the population at increased risk of reduced BMD compared to the base case. Not only does the risk of fracture increase, the risk increases post-treatment compared to pre-treatment which suggests vitamin D does not prevent reduced BMD which questions the validity of the regression equation when used to inform the model (Table 66). One plausible reason for this is that the regression equation was based on a population with secondary osteoporosis, who would have a lower BMD than children and young people at increased risk of reduced BMD; as a result the pre-treatment BMD used in the equation is too large enough to increase the post-treatment to demonstrate an improvement. For this reason, the regression is unreliable in alternative populations to participants in the primary study. Consequently, vitamin D is dominated by cycling and “no treatment” under this scenario as it is now less effective. Vitamin D also no longer dominates vibration therapy and becomes a decision of disinvestment. In all remaining comparisons, the resulting decision is unchanged.
When considering the impact of the regression equation in the proven osteoporosis population, the risk of fracture for vitamin D is increased (27.8% vs. 28.0%) whereas the risk of fracture for risedronate plus vitamin D is reduced (27.2% vs. 26.8%). Despite this the resulting decisions do not change.
Scenario 5. Cost of standing frame equipment
Varying the cost of a standing frame does not impact the resulting decision as the ICER remains above NICE’s cost-effective threshold.
Scenario 6. Cost of vibration equipment
Varying the cost of a vibration equipment does not impact the resulting decision as the ICER remains above NICE’s cost-effective threshold.
Scenario 7. Zero active exercise equipment cost
Applying no equipment costs to active exercise reduced the total cost of cycling, but this does not impact the resulting decision. For the comparison F1 vs. lumbar spine, cycling now dominates “no treatment” where it was previously more effective and more expensive with an ICER of £6,261, but in both cases cycling would be considered cost-effective relative to “no treatment”.
Summary
Overall, the comparisons have proven to be robust to the sensitivity analysis undertaken, i.e. the resulting decision does not change. One exception was the comparison between cycling (lumbar spine) and “no treatment” (F1); however the validity of this particular comparison using different BMD is questionable given that comparisons using equivalent sites (F1 vs. F1, or lumbar vs. lumbar) were not sensitive to the scenarios undertaken.
G.9.9.3. Probabilistic sensitivity analysis (PSA)
Comparisons of interest in the population at increased risk of reduced BMD are limited to vitamin D plus calcium vs. “no treatment”, and cycling vs. “no treatment”, and in the proven osteoporosis population risedronate plus vitamin D vs. pamidronate disodium. For the reasons described in Section G.9.9.1, only comparisons of equivalent BMD sites (i.e. F1 vs. F1 or lumbar spine vs. lumbar spine) will be presented here.
Population at increased risk of reduced BMD
Intervention: Vitamin D plus calcium
It is evident from Figure 8 and Figure 9 that all simulations predict vitamin D plus calcium to be cost-effective relative to “no treatment” under a threshold of £20,000 per QALY.
Moreover, assuming a WTP threshold of £20,000 or £30,000 per QALY there is a 100% probability that calcium plus vitamin D is optimal.
Vitamin D plus calcium has a deterministic input in PSA as the probability of fracture cannot fall below 0%. For this reason almost all simulations find calcium plus vitamin D to be more effective than “no treatment”.
Figure 8CEAC, vitamin D plus calcium (lumbar spine) vs. “no treatment” (lumbar spine)
WTP, willingness-to-pay
Intervention: active exercise (cycling)
With regards to cycling, the simulations in Figure 11 are distributed across all 4 quadrants of the cost-effectiveness plane, and almost half of simulations (46%) at a WTP threshold of £20,000 per QALY predict cycling to be cost-effective relative to “no treatment” when F1 sites are compared. As a result this questions if the deterministic ICER of £95,401 is overestimated. However, assuming a WTP threshold of £20,000 or £30,000 the probability that cycling is optimal is never greater than “no treatment” (Figure 10). Overall, the underlying probability distributions included in PSA are arbitrary due to insufficient data to estimate confidence intervals, also questioning their reliability.
Figure 10CEAC, cycling (F1) vs. “no treatment” (F1)
CEAC, cost-effectiveness acceptability curve; WTP, willingness-to-pay
Figure 11CE plane, 1,000 simulations, cycling (F1) vs, “no treatment” (F1)
QALYs, quality-adjusted life years; WTP, willingness-to-pay
When lumbar sites are compared in Figure 12 and Figure 13, the majority of simulations lie in the north-west quadrant, reflecting the base case where cycling is dominated by “no treatment”. Specifically, cycling is considered cost-effective relative to “no treatment” in 28% of simulations.
Simulations that are more expensive are generally less effective, this is because poor QALY gains are associated with the cost of fracture treatment; hence, the inverse relationship between QALYs and costs is to be expected in Figure 11 and Figure 13.
The simulations from both comparisons reflect the base-case uncertainty surrounding the chosen BMD sites, but the PSA has demonstrated that the cost-effectiveness of cycling may be more nuanced than implied by the deterministic results.
Figure 12CEAC, cycling (lumbar) vs. “no treatment” (lumbar)
CEAC, cost-effectiveness acceptability curve; WTP, willingness-to-pay
Proven osteoporosis
All simulations in Figure 16 predict pamidronate disodium to be more expensive than risedronate plus vitamin D. In terms of drug treatment costs, risedronate plus vitamin D is a lot cheaper than pamidronate disodium (£601 vs. £7,103 /year) so it reasonable for none of the simulations to lie in the south quadrants. As a result, the probability of fracture or the cost of treating fractures would have to be a lot larger for risedronate plus vitamin D to have a greater total cost than pamidronate disodium.
In addition, pamidronate disodium is almost always shown to be more effective than risedronate plus vitamin D in Figure 16, with the majority of simulations lying in the (north-) east quadrant. This is reasonable because pamidronate disodium is always associated with a lower probability of fracture (where a fracture is associated with a disutility) than risedronate plus vitamin D (Figure 14). Overall, pamidronate disodium would not be considered cost-effective in any of the simulations under a £20,000 WTP threshold as the simulated ICER’s are much greater than this.
At all feasible WTP thresholds the probability that pamidronate disodium is optimal is zero (Figure 15).
Figure 15CEAC, pamidronate (F1) vs. risedronate plus vitamin D (F1)
CEAC, cost-effectiveness acceptability curve; WTP, willingness-to-pay
Postural management
In Figure 17, the standing frame is cost-effective relative to “no treatment” in 0% of simulations. Similarly, Figure 18 illustrates that at a WTP threshold of £20,000, or £30,000 the probability that the standing frame is cost-effective is zero.
Figure 17CE plane, 1,000 simulations, standing frame vs. “no treatment”
QALYs, quality-adjusted life years; WTP, willingness-to-pay
G.9.10. Discussion
The probability of fracture was based on Henderson 2010 who estimated this for 4 BMD sites: the lumbar spine, and the 3 regions of the distal femur. However, not all studies reported those exact sites; hence a number of assumptions were made to include a number of interventions in the model (Section G.9.3.2). Consequently, the risk of fracture may underestimate or overestimate the risk of fracture for some interventions, but the direction of this effect is unknown. Furthermore, Henderson 2010 did not report the time horizon their prevalence data reflected.
Adjustments were made to the BMD values in the model to reflect a homogenous population as it was evident studies included participants functioning at different levels (Section G.9.3.3). External consistency was assessed by comparing the estimated probabilities of fracture against the clinical evidence review. Following this comparison, it was accepted that the improvements post-treatment were preserved following those adjustments made in the model. For example, studies that reported a significant difference in the clinical evidence review were associated with a lower probability of fracture than studies that did not report a significant difference.
The model also demonstrated that comparing interventions at different sites favoured the intervention with BMD measured from the distal femur, as the lumbar spine was associated with a larger risk of fracture given the same Z-score – studies did not produce lower Z-scores for the lumbar spine to compensate for this.
For the reasons outlined above, this model would benefit from a study that compared the BMD at both the distal femur and lumbar spine as the clinical evidence review demonstrated that different sites can lead to different results (Section G.9.3.2); or ideally, a study that assessed the prevention of fractures in children and young people with cerebral palsy, to remove the uncertainty in transforming a BMD measure into a risk of fracture.
The interventions within a population were found to have similar fracture risks, hence the small changes in the risk of fracture, pre- and post- treatment (Section G.9.3.5). Consequently, an important driver of cost-effectiveness between comparisons was treatment costs. However, it was evident that expensive interventions, particularly vibration therapy, could not be justified by providing additional benefits over their comparators. In addition, it is important to consider if all health gains have been captured. The Committee noted that administering pamidronate disodium as an inpatient procedure over 2 days would cause the child or young person with cerebral palsy a lot of inconvenience, and some active interventions can cause pain.
The Committee highlighted that the type of fractures children and young people with cerebral palsy incur from reduced BMD varies hugely, ranging from minor fractures of the foot, to fractures of the femur and vertebrae, which can involve complications that incur large costs and significantly impair quality of life. It was also noted that fractures can go unrecognised incurring zero treatment costs. In the model it is assumed a child or young person with cerebral palsy can have 1 fracture over the time horizon in the model; however, it is possible for them to experience more than 1 fracture in clinical practice.
Henderson 2010 stated that in children and young people with cerebral palsy, over half of all fractures occur in the lower limb or femur. For this reason a base case informed by a severe fracture was reasonable and a minor fracture was explored as a sensitivity analysis (Section G.9.9.2).
Costing the equipment for interventions was difficult due to the number of manufacturers and models that are available (Section 64G.9.6). However, this was explored through sensitivity analysis, where the cost of the standing frame and vibration equipment was increased and decreased by 50% and the cost of active exercise equipment was set to zero (Section G.9.7.1 and Section G.9.9.2). The results from these analyses suggested that equipment costs were not an important driver of results; hence this was not considered as a severe limitation.
Caulton 2004 investigated the use of standing frame compared to no increase in the regular standing duration in their trial. However, the comparison analysed in the model was between a standing frame and no standing frame as this comparison was of greater interest to the Committee, particularly when standing frames are not already in possession and require an upfront payment. Consequently, the clinical effectiveness of standing frames may be underestimated in the model.
Unfortunately we cannot tell if calcium is causing the difference in cost-effectiveness between vitamin D with and without calcium because no clinical effectiveness data was identified for calcium alone.
G.9.11. Conclusion
Vibration therapy would not be considered cost-effective to limit reductions in BMD in a population at increased risk of reduced BMD as it has an ICER substantially above NICE’s cost-effective threshold, this also holds when the cost of the equipment is reduced by 50%. However, it is important to note that vibration therapy could be considered cost-effective for indications that are beyond the scope of this model.
The cost-effectiveness of cycling in a population at increased risk of reduced BMD was highly uncertain and driven by the BMD site used to estimate clinical effectiveness. However, if health care professionals are not required to supervise active exercise, and active exercise is something children and young people with cerebral palsy choose to do and enjoy, this should be encouraged, as there would be negligible opportunity costs to consider.
Vitamin D and Vitamin D plus calcium would be regarded as cost-effective interventions compared to “no treatment” in a population at increased risk of reduced BMD. However, the risk of fracture post-treatment for vitamin D plus calcium may be overestimated in the model as the trial used to inform clinical effectiveness included participants with proven osteoporosis, who had the potential for greater improvements in BMD than participants without osteoporosis. For this reason, the benefits of supplementation may outweigh the costs in children and young people at high risk of reduced BMD with inadequate levels.
Risedronate plus vitamin D would be considered cost-effective relative to pamidronate disodium, but whether the ICER compared to pamidronate disodium lies in the south-east quadrant (dominant) or south-west quadrant (less expensive and less effective) depends on the site of BMD used to estimate clinical effectiveness. Moreover, pamidronate disodium would not be considered cost-effective in a proven osteoporosis population, regardless of its comparator as the relative gains in effectiveness do not outweigh the additional cost.
The standing frame would not be considered cost-effective to prevent reduced BMD as the ICER is substantially higher than NICE’s threshold, this also holds when the cost of the equipment is reduced by 50%. However, it is important to note that standing frames may be considered cost-effective for other purposes. Furthermore, if children and young people with cerebral palsy already possess a standing frame, its use should not be discouraged.
The Committee’s discussion regarding the associated economic benefits and harms are reported in the Section 19.6.3 ‘Evidence to recommendations’.
G.9.12. Supplementary tables
Table 64Adjustments to estimate post-treatment values
| Population | Intervention | Post-treatment BMD, unadjusted | Inflator calculation: baseline pretreatment BMD (Table 36) / study reported pre-treatment BMD (Table 35) | Inflator | Post-treatment BMD, adjusted (Table 39) |
|---|---|---|---|---|---|
| At increased risk of reduced BMD | Active exercise (cycling) | Lumbar spine: 0.58 F1: 0.74 | NA | NA | NA |
| Weight-bearing activity | Lumbar spine: NR F1: 0.38 | F1: 0.72/0.36 | F1: 2.00 | F1: 0.76 | |
| Vitamin D | Lumbar spine: NR F1: 0.33 a | F1: 0.72/0.32 | F1: 2.25 | F1: 0.74 | |
| Vitamin D & calcium | Lumbar spine: 0.48 F1: NR | Lumbar spine: 0.58/0.38 | Lumbar spine: 1.53 | Lumbar spine: 0.73 | |
| Vibration therapy | Lumbar spine: 0.50 F1: 0.63 | Lumbar spine: 0.72/0.49 F1: 0.58/0.60 | Lumbar spine: 1.18 F1: 1.22 | Lumbar spine: 0.59 F1: 0.77 | |
| “No treatment” b | Lumbar spine: 0.58 F1: 0.73 | NA | NA | NA | |
| Proven osteoporosis | Pamidronate disodium | Lumbar spine: 0.43 c F1: 0.63 c | NA | NA | NA |
| Vitamin D & calcium | Lumbar spine: 0.48 F1: NR | Lumbar spine: 0.32/0.38 | Lumbar spine: 0.83 | Lumbar spine: 0.40 | |
| Risedronate & vitamin D | Lumbar spine: NR F1: 0.48 a | F1: 0.35/0.45 | F1: 0.78 | F1: 0.38 | |
| Vitamin D | Lumbar spine: NR F1: 0.33 a | F1: 0.35/0.32 | F1: 1.09 | F1: 0.36 | |
| Postural management | Standing frame | Lumbar spine: 0.238 F1: NR | NA | NA | NA |
| “No treatment” | Lumbar spine: 0.149 F1: NR | NA | NA | NA |
BMD, bone mineral density; NA, not applicable; NR, not reported
- (a)
Estimated from reported regression line described in Section G.9.3.3
- (b)
Taken from cycling no treatment arm
- (c)
Calculated from reported Z-scores
Table 65Population at increased risk of reduced BMD, base case results (ICER)
| Intervention ▼ vs. ▶ | Cycling | Weight-bearing exercise | Vitamin D | Vitamin D + calcium | Vibration therapy | “No treatment” | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| F1 | L | F1 | L | F1 | L | F1 | L | F1 | L | F1 | Lumbar | ||
| Cycling | F1 | - | Dominated a | NC | Dominated b | NC | NC | Dominated c | £3,104,67 9 (SW) d | £969,648 (SW) d | £95,041 (NE) | £6,261 (NE) | |
| L | Dominated a | NC | Dominated b | NC | NC | Dominated c | £52,606,6 91 (SW) d | £1,402,49 4 (SW) d | Dominated e | Dominated e | |||
| Weightbearing exercise | F1 | Dominant f | Dominant f | - | Dominant g | NC | NC | Dominated h | Dominant i | Dominant i | Dominant j | Dominant j | |
| L | NC | NC | NC | NC | NC | NC | NC | NC | NC | NC | |||
| Vitamin D | F1 | Dominant k | Dominant k | Dominated l | NC | - | NC | Dominated m | £3,654,15 6 (SW) n | Dominant o | Dominant p | Dominant p | |
| L | NC | NC | NC | NC | NC | NC | NC | NC | NC | NC | |||
| Vitamin D plus calcium | F1 | NC | NC | NC | NC | NC | NC | - | NC | NC | NC | NC | |
| L | Dominant q | Dominant q | Domina nt r | NC | Dominant s | NC | Dominant t | Dominant t | Dominant u | Dominant u | |||
| Vibration therapy | F1 | £3,104,67 9 (NE) | £969,648 (NE) | Dominated v | NC | £3,654,15 6 (NE) | NC | NC | Dominated x | - | £2,044,94 7 (NE) | £1,154,538 (NE) | |
| L | £52,606,6 91 (NE) | £1,402,49 4 (NE) | Dominated v | NC | Dominated w | NC | NC | Dominated x | £5,288,63 2 (NE) | £1,791,107 (NE) | |||
BMD, bone mineral density; ICER, incremental cost-effectiveness ratio; NE, north-east quadrant; NC, not calculable; SW, south-west quadrant South-west ICERs represent the costs saved per QALY loss
- (a)
Cycling more expensive and less effective than weights
- (b)
Cycling more expensive and less effective than vitamin D
- (c)
Cycling more expensive and less effective than calcium plus vitamin D
- (d)
Cycling less expensive and less effective than vibration therapy
- (e)
Cycling more expensive and less effective than “no treatment”
- (f)
Weights less expensive and more effective than cycling
- (g)
Weights less expensive and more effective than vitamin D
- (h)
Weights more expensive and less effective than calcium plus vitamin D
- (i)
Weights less expensive and more effective than vibration therapy
- (j)
Weights less expensive and more effective than “no treatment”
- (k)
Vitamin D less expensive and more effective than cycling
- (c)
Vitamin D more expensive and less effective than weights
- (d)
Vitamin D more expensive and less effective than calcium plus vitamin D
- (e)
Vitamin D less expensive and less effective than vibration therapy
- (f)
Vitamin D less expensive and more effective than vibration therapy
- (g)
Vitamin D less expensive and more effective than “no treatment”
- (h)
Vitamin D plus calcium less expensive and more effective than cycling
- (i)
Vitamin D plus calcium less expensive and more effective than weights
- (j)
Vitamin D plus calcium less expensive and more effective than vitamin D
- (k)
Vitamin D plus calcium less expensive and more effective than vibration therapy
- (l)
Vitamin D plus calcium less expensive and more effective than “no treatment”
- (m)
Vibration therapy more expensive and less effective than weights
- (n)
Vibration therapy more expensive and less effective than vitamin D
- (o)
Vibration therapy more expensive and less effective than calcium plus vitamin D
- (p)
Vitamin D less expensive and more effective than “no treatment”
Table 66Scenario 4, resulting BMD and Z-scores
| Intervention, population | Pre-treatment BMD, adjusteda | Post-treatment BMD, base case | Post-treatment BMD, regression equation | Post-treatment Z-score, base case | Post-treatment Z-score, regression equation | Probability of fracture, base case | Probability of fracture, regression equation |
|---|---|---|---|---|---|---|---|
| Vitamin D, at increased risk of reduced BMD | 0.72 | 0.74 | 0.69b | -0.18 | -0.64 | 10.8% | 12.8% |
| Vitamin D, proven osteoporosis | 0.35 | 0.36 | 0.36c | -3.91 | -3.94 | 27.8% | 28.0% |
| Risedronate plus vitamin D, proven osteoporosis | 0.35 | 0.38 | 0.39d | -3.79 | -3.69 | 27.2% | 26.8% |
- (a)
Used to calculate post-treatment bone mineral density (BMD) in the base case and the regression equation
- (b)
0.9×0.72 + 0.042
- (c)
0.9×0.35 + 0.042
- (d)
0.952×0.35 + 0.056
Table 67PSA parameters
| Parameter | Distribution | μ | σ | Source |
|---|---|---|---|---|
| Total treatment costs | ||||
| Active exercise (cycling) | Gamma | £133 | £27 | Assumption, SD = 20% of the mean |
| Weight-bearing exercise | £90 | £18 | ||
| Vitamin D | £63 | £13 | ||
| Vitamin D & calcium | £115 | £23 | ||
| Vibration therapy | £4,682 | £936 | ||
| Pamidronate disodium | £7,103 | £1,421 | ||
| Risedronate & vitamin D | £601 | £120 | ||
| Standing frame | £4995 | £999 | ||
| “No treatment” | £30 | £6 | ||
| Fracture | £7,104 | £1,420 | ||
| Utility | ||||
| GMFCS level II, no fracture | Beta | 0.50 | 0.20 | Rosenbaum 2007 |
| GMFCS level III, no fracture | 0.39 | 0.31 | ||
| GMFCS level IV, no fracture | 0.16 | 0.21 | ||
| Disutility from fracture | ||||
| Utility multiplier | Beta | 0.6 | 0.012 | Assumption, SD = 20% of the mean |
| Utility multiplier | 0.7 | 0.014 | ||
| Utility multiplier | 0.8 | 0.016 | ||
| Probability of fracture | ||||
| First line | ||||
| Active exercise (cycling), F1 | Beta | 10.9% | 2.18% | Assumption, SD = 20% of the mean |
| Active exercise (cycling), lumbar spine | 12.6% | 2.52% | ||
| Weight bearing activity, F1 | 10.1% | 2.02% | ||
| Vitamin D, F1 | 10.8% | 2.16% | ||
| Vitamin D & calcium, lumbar spine | 0.1% | 0.00% | ||
| Vibration therapy, F1 | 7.1% | 1.42% | ||
| Vibration therapy, lumbar spine | 10.8% | 2.16% | ||
| “No treatment”, F1 | 11.3% | 2.26% | ||
| “No treatment”, lumbar spine | 12.1% | 2.42% | ||
| Proven osteoporosis | ||||
| Vitamin D, F1 | Beta | 27.8% | 5.56% | Assumption, SD = 20% of the mean |
| Vitamin D & calcium, lumbar spine | 31.7% | 6.34% | ||
| Risedronate plus vitamin D, F1 | 27.2% | 5.44% | ||
| Pamidronate disodium, F1 | 18.2% | 3.64% | ||
| Pamidronate disodium, lumbar spine | 28.7% | 5.74% | ||
| Postural management | ||||
| Standing frame, lumbar spine | Beta | 30.6% | 6.12% | Assumption, SD = 20% of the mean |
| “No treatment” | 32.9% | 6.58% | ||
PSA, probabilistic sensitivity analysis; SD, standard deviation
Table 68Philips checklist, BMD
| Dimension of quality | Comments |
|---|---|
| Structure | |
| S1: Statement of decision problem/objective | Clearly stated. |
| S2: Statement of scope/perspective | Clearly stated perspective (UK NHS). |
| S3: Rationale for structure | Clearly stated. Intermediate outcomes (BMD) were transformed into a risk of fracture that can be assigned a utility value and treatment cost. This final outcome is consistent with the benefits of treatment as preventing reduced BMD should reduce the risk of fracture. A decision tree was appropriate to represent outcomes of treatment (fracture vs. no fracture), and time did not need to be defined. |
| S4: Structural assumptions | The structure of the model was discussed with the Guideline Committee who accepted and informed some of the structural assumptions of the model. These are reasonable given the available data – this is why both DEXA sites were included sometimes they only reported one or the other. Also, assumptions have been addressed in the sensitivity analysis. |
| S5: Strategies/ comparators | All feasible comparisons were presented in the Appendix, and the write-up focused on the comparisons of most interest to the Committee for each of the 3 populations. Strategies employed are adequate and uncertainty on parameter values were justified or explored in sensitivity analysis. |
| S6: Model type | Appropriate; cost-utility analysis. |
| S7: Time horizon | Appropriate: 1 Year (The time horizon for the model was a year as this reflected the longest trial follow-up in the clinical evidence review, following this no discount rate was applied). There is an option in the model to vary the time horizon but it is unclear how the probability of fracture is influenced. It is also unclear how the probability has been adjusted to reflect the time horizon in the model. However the limitations of the source were described. |
| S8: Disease states/pathways | Appropriate; Decrease in BMD leading to fractures clearly stated and visible in analysis |
| S9: Cycle length | Appropriate; no cycle length as not necessary for decision tree analyses. |
| Data | |
| D1: Data identification | Systematic reviews were not undertaken to identify costs, utilities or the risk of fracture; however sources have been justified and the methods used to identify sources is transparent. Used credible sources specified in the Guidelines manual (NHS Reference Costs, Drug Tariff, PSSRU) where data could not be identified Guideline committee opinion was sought. Given the objective of the model – to identify cost effective interventions that reduce the risk of reduced BMD in children and young people with CP – the data identified is appropriate because, where possible, the sources matched the intended population. For data that did not match the intended population, justification for the use of this data was provided by the committee. It is clear that particular attention was paid to identifying the data for the parameters (cost of treatment, cost of fractures, probability of fracture, and quality of life impact of fractures) which the results were particularly sensitive to uncertain parameters were varied in sensitivity analysis. Instead of providing data, the committee suggested how the sources of data could be modified to inform the model/population. For example they advised on the cost |
| D2: Pre-model data analysis | All data modelling methodology should is described and based on justifiable statistical and epidemiological methods and:
|
| D2a: Baseline data | The methodology for deriving baseline (probability of fracture) data, for both pre and post treatment, was appropriate Using a study by Henderson 2010, based on identifying a correlation between DEXA BMD values and the probability of fracture (in children and adolescents with CP and Muscular Dystrophy), trends (regression) lines were estimated (by plotting z-score values for BMD against probability values). Estimating trends allowed differences in treatment effects to be seen; no difference would be demonstrated if the range of z-scores in the study was used. Each line of regression represented this relationship for a different anatomical region (F1, F2, F3, and Lumbar Spine). Use of this study, for the derivation of the probabilities, was justified seeing as the population the study was based on was similar to that in the model. The FRAX tool for deriving the probabilities of fractures, on the other hand, was deemed unsuitable because it’s based on post-menopausal women. It was noted in the report, however, that the GMFCS group (IV to V) included in Henderson 2010 is a high-risk group, in terms of the risk of reduced BMD, and therefore the probability figures derived would be overestimated when applied to those in a lower GMFCS group (like some members of the population within the model). For each population within the model, unilateral pre-treatment BMD figures were taken from a single study. This was done to address the issue of heterogeneity within the sources. The post-treatment BMD values for each intervention) were obtained from studies within the clinical evidence review (data for each intervention came from a separate study). Some studies, however, did not have post treatment BMD figures, but had sufficient information (p values, graphs) that allowed assumptions to be made from which BMD values were derived. Without these assumptions, these interventions (standing frame, risedronate and vitamin D) could not be incorporated into the model. Furthermore, in some studies where post-treatment BMD figures were published, some of these figures had to be adjusted (inflated) as the pre-treatment BMD values they were dependent on were also adjusted (inflated) to match the unilateral pre-treatment values of BMD previously mentioned. Using expected values of BMD (for which the method of derivation was also stated and justified), z-scores were calculated for pre and post treatment values of BMD and the corresponding probabilities, from the regression lines, were obtained and used as baseline data. |
| D2b: Treatment effects | The key measure of effectiveness modelled by the committee was the change (decrease) in the probability of fracture; dependant on the change (increase) in the BMD. The method with which the probability of fractures is calculated, within the model, in relation to BMD figures is discussed in D2a. The meta-analysis of relative treatment effects is irrelevant in this model as each trial study concerns a different intervention. Assumptions regarding the continuing effect of treatments once they have ceased are not discussed within this model. This may be due to the time horizon being 1 year whilst treatments for BMD, such as standing frames, are required for multiple years. Alternative assumptions for risedronate and vitamin D based on a regression equation to estimate treatment effects in the study was explored in sensitivity analysis. |
| D2c: Costs | The latest sources of data were where possible (NHS Reference Costs 2014/15, electronic drug tariff 2015) and inflated costs to the year 2015 (for example: Administration costs incurred by pamidronate disodium taken from TA265, Section G.9.6.2). The sources for all costs incorporated into the model are clearly stated. All costs are broken down into their different contributing factors which are also costed. The costs of non-pharmacological equipment were treated as capital costs and were therefore accounted for using the annual equivalent cost method. (Section G.9.6). Justification is provided by the committee whenever proxies are used. For example, the committee notes that it would be reasonable to use ICD HRG codes relating to hip traumas as a proxy for femur fractures which were not in HRG codes related to a fracture diagnosis. The same proxy relationship (hip in place of femur) was used for the cost of femur procedures. It was also noted that ‘no treatment’ would actually still incur costs and this was also justified by the committee. It was stated costing the equipment was difficult due to the number of manufacturers and models available. However this was explored through sensitivity analysis where the cost of equipment was increased and decreased by 50%. |
| D2d: Quality of life weights (utilities) | The utilities incorporated into the model are appropriate for the decision problem. Utility values for living with CP were calculated using a study from Rosenbaum 2007 in which the carers of individuals diagnosed with CP completed a quality of life survey on behalf of the patients. It was also noted that this method of gathering utility data goes against the NICE reference case – which states that the patients themselves should assess their own quality of life using EQ-5D – but in the absence of alternative values this study was chosen. Utility values for experiencing a fracture in addition to living with CP were calculated using multipliers to discount the original utility values. It was noted that this was based on NICE data regarding an older population of women with hip and vertebral fractures; although the multipliers were revised to account for lower limb fractures in children. Also, justification was provided as to the GMFCS levels assigned to each of the populations. |
| D3: Data incorporation | Appropriate; data was incorporated logically and reasonably. Sources were described and referenced in sufficient detail. The process of data incorporation was transparent to enable another modeller to replicate the results. Further details were provided in the appendix to estimate several inputs and distributions for PSA. |
| Assessment of uncertainty | |
| D4a: Methodological | Appropriate (PSA and scenario analysis). |
| D4b: Structural | Appropriate; scenario analyses undertaken using values that reflect real life estimates and with rationale described e.g. the committee opinion on the utility of GMFCS level IV. Also, a scenario using a regression line for the risedronate and vitamin D study to estimate the treatment effect on BMD was included. |
| D4c: Heterogeneity | Appropriate; model was run separately for each population. A baseline adjustment was used and results were included for the different populations;
|
| D4d: Parameter | Appropriate; uncertainty was assessed through deterministic and probabilistic sensitivity analysis. Scenario analysis varying the cost of a standing frame based on the different available models and manufacturers was included in model and justified. However, the underlying probability distributions were unknown for the majority of parameters varied in PSA. An arbitrary starting point for unknown data was to assume the value of the standard deviation will be 20% which questions the reliability of this analysis. |
| Consistency | |
| C1: Internal consistency | Internal validity was assessed by the primary modeller, and a second health economist. The following areas of the model were checked:
|
| C2: External consistency | External consistency was assessed by assessing the face validity of the model, and comparing the results of the analysis against the clinical evidence review and other published data (cross validation). An explanation was also provided for the questionable results for post-treatment probability of fracture (0%) for the vitamin D + calcium intervention. |
BMD, bone mineral density; CP, cerebral palsy; DEXA, dual energy X-ray absorptiometry; EQ-5D, European quality of life-5 dimensions; CYP, children and young people; FRAX, fracture risk assessment tool; GMFCS, Gross Motor Function Classification System; HRG, Healthcare resource group; ICD, International Statistical Classification of Diseases and Related Health Problem; ICER, incremental cost-effectiveness ratio; PSA, probabilistic sensitivity analysis; QALY, quality adjusted life year.
- Literature review
- Assessment of eating, drinking and swallowing difficulties
- Management of eating, drinking and swallowing difficulties
- Optimising nutritional status
- Management of pain, distress and discomfort
- Managing sleep disturbance in children and young people with cerebral palsy
- Managing mental health problems in children and young people with cerebral palsy
- In children and young people with cerebral palsy, what interventions are cost-effective in optimising saliva control?
- Prevention of reduced bone mineral density
- Health Economics - Cerebral palsy in under 25s: assessment and managementHealth Economics - Cerebral palsy in under 25s: assessment and management
Your browsing activity is empty.
Activity recording is turned off.
See more...